J Cerebrovasc Endovasc Neurosurg.
2015 Sep;17(3):234-238. 10.7461/jcen.2015.17.3.234.
Huge Intramural Hematoma in a Thrombosed Middle Cerebral Artery Aneurysm: A Case Report
- Affiliations
-
- 1Department of Neurosurgery, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea. md@medimail.com
- 2Department of Radiology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea.
- KMID: 2069249
- DOI: http://doi.org/10.7461/jcen.2015.17.3.234
Abstract
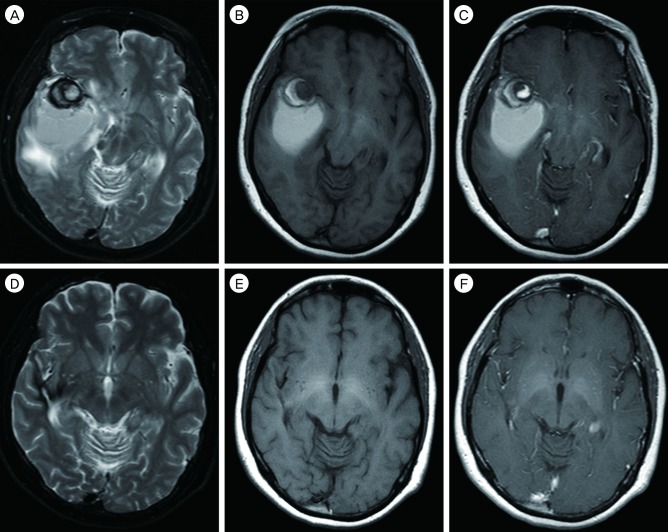
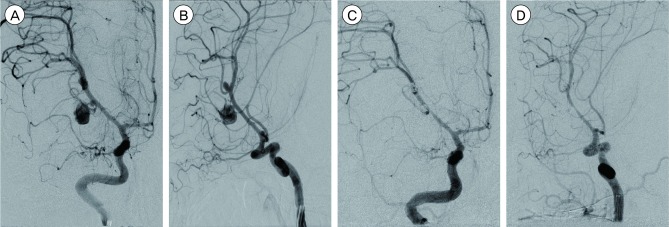
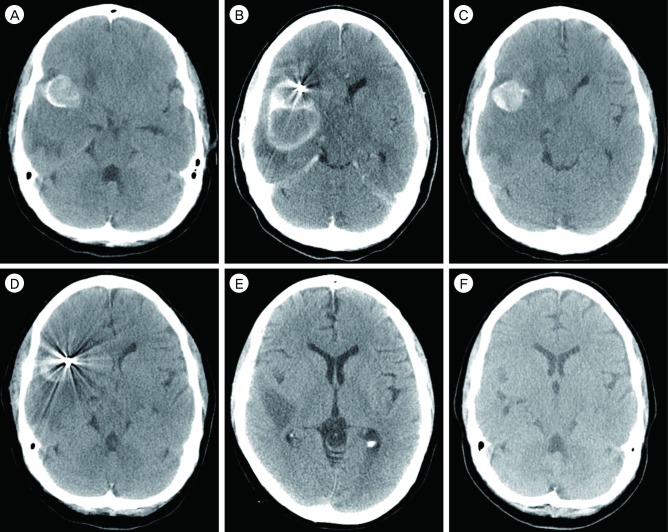
- We describe a case of a huge intramural hematoma in a thrombosed middle cerebral artery aneurysm. A 47-year-old female patient with liver cirrhosis and thrombocytopenia presented to the neurosurgical unit with a 5-day history of headache and cognitive dysfunction. Magnetic resonance imaging and computed tomography of the brain showed a thrombosed aneurysm located in the right middle cerebral artery with a posteriorly located huge intramural hematoma mimicking an intracerebral hematoma. Imaging studies and cerebrospinal fluid analysis showed no evidence of subarachnoid hemorrhage. Angiography showed a partially thrombosed aneurysm at the origin of the right anterior temporal artery and an incidental aneurysm at the bifurcation of the right middle cerebral artery. Both aneurysms were embolized by coiling. After embolization, the thrombosed aneurysmal sac and intramural hematoma had decreased in size 4 days later and almost completely disappeared 8 months later. This is the first reported case of a nondissecting, nonfusiform aneurysm with a huge intramural hematoma, unlike that of a dissecting aneurysm.
MeSH Terms
Figure
Cited by 1 articles
-
Staged hybrid treatment for giant thrombosed fusiform aneurysm
Yunho Noh, Sung Ho Lee, Seok Mann Yoon, In Hag Song, Jae Sang Oh
J Cerebrovasc Endovasc Neurosurg. 2021;23(4):359-364. doi: 10.7461/jcen.2021.E2021.06.004.
Reference
-
1. El Beltagy M, Muroi C, Imhof HG, Yonekawa Y. Peripheral large or giant fusiform middle cerebral artery aneurysms: report of our experience and review of literature. Acta Neurochir Suppl. 2008; 103:37–44. PMID: 18496943.2. Horie N, Takahashi N, Furuichi S, Mori K, Onizuka M, Tsutsumi K, et al. Giant fusiform aneurysms in the middle cerebral artery presenting with hemorrhages of different origins. Report of three cases and review of the literature. J Neurosurg. 2003; 8. 99(2):391–396. PMID: 12924715.3. Krings T, Choi IS. The many faces of intracranial arterial dissections. Interv Neuroradiol. 2010; 6. 16(2):151–160. PMID: 20642889.
Article4. Krings T, Lasjaunias PL, Geibprasert S, Pereira V, Hans FJ. The aneurysmal wall. The key to a subclassification of intracranial arterial aneurysm vasculopathies? Interv Neuroradiol. 2008; 9. 14(Suppl 1):39–47. PMID: 20557772.5. Krings T, Piske RL, Lasjaunias PL. Intracranial arterial aneurysm vasculopathies: targeting the outer vessel wall. Neuroradiology. 2005; 12. 47(12):931–937. PMID: 16136262.
Article6. Mrak G, Paladino J, Stambolija V, Nemir J, Sekhar LN. Treatment of giant and large fusiform middle cerebral artery aneurysms with excision and interposition radial artery graft in a 4-year-old child: case report. Neurosurgery. 2014; 3. 10(Suppl 1):E172–E177. discussion E177PMID: 24509498.
Article7. Nagahiro S, Takada A, Goto S, Kai Y, Ushio Y. Thrombosed growing giant aneurysms of the vertebral artery: growth mechanism and management. J Neurosurg. 1995; 5. 82(5):796–801. PMID: 7714605.
Article8. Sagoh M, Hirose Y, Murakami H, Akaji K, Katayama M, Hayashi T. Late hemorrhage from persistent pseudoaneurysm in vertebral artery dissection presenting with ischemia: case report. Surg Neurol. 1999; 11. 52(5):480–483. discussion 483-4. PMID: 10595768.
Article9. Yasui T, Sakamoto H, Kishi H, Komiyama M, Iwai Y, Yamanaka K, et al. Rupture mechanism of a thrombosed slow-growing giant aneurysm of the vertebral artery-case report. Neurol Med Chir (Tokyo). 1998; 12. 38(12):860–864. PMID: 10063360.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Subdural Hematoma Due to Ruptured Intracerebral Aneurysm
- Intracranial Mycotic Aneurysm: Case Report
- Subarachnoid Hemorrhage Due to a Ruptured Middle Cerebral Artery Bifurcation Aneurysm Superimposed by an Idiopathic Intracerebral Hematoma
- Duplication of the Middle Cerebral Artery: Case Report
- Thrombosed Large Middle Cerebral Artery Aneurysm Mimicking an Intra-Axial Brain Tumor: Case Report and Review of Literature