J Korean Soc Radiol.
2015 Oct;73(4):230-239. 10.3348/jksr.2015.73.4.230.
Intra-Arterial Therapy for Cardioembolic Internal Carotid Artery Terminus Occlusion: The Past and Present Status in Real Practice
- Affiliations
-
- 1Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Korea. jck0097@gmail.com
- 2Department of Neurology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 3Department of Radiology, Myongji Hospital, Goyang, Korea.
- 4Department of Radiology, Chungbuk National University College of Medicine, Daejeon, Korea.
- KMID: 2068713
- DOI: http://doi.org/10.3348/jksr.2015.73.4.230
Abstract
- PURPOSE
There is little data on the effect of intra-arterial therapy (IAT) in acute cardioembolic internal carotid artery terminus (ICAT) occlusion that has poor prognosis. We determined procedural and clinical outcomes in patients with acute cardioembolic ICAT occlusion treated with different methods of IAT.
MATERIALS AND METHODS
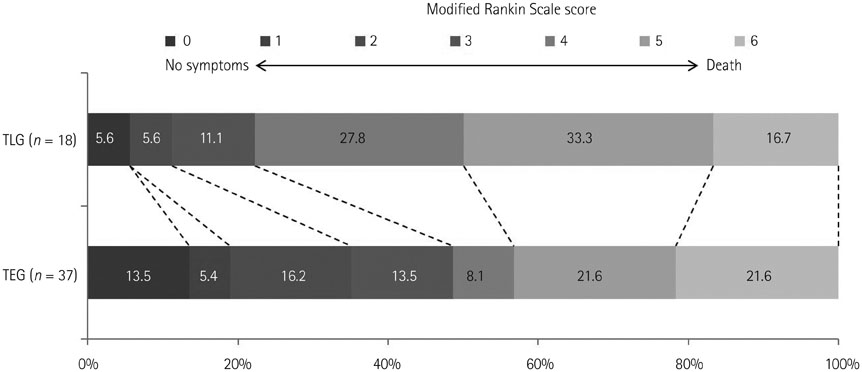
On retrospective review of our registry, patients with cardioembolic ICAT occlusion were categorized as thrombolytic-based IAT group (TLG) and thrombectomy-based IAT group (TEG) according to the primary endovascular technique. Subsequently, procedural and clinical outcomes were compared.
RESULTS
Fifty-five patients had cardioembolic ICAT occlusion and 18 patients were assigned to TLG and 37 patients to TEG. The rate of complete reperfusion was significantly higher and the groin puncture to reperfusion time was significantly shorter in TEG than those in TLG. There was a trend towards functional outcome at 3 months in the TEG group; however, it was not statistically significant (p = 0.06). Age, baseline Albert Stroke program early CT score and puncture to reperfusion time were factors affecting unfavorable outcome at 3 months, on multivariable analysis.
CONCLUSION
Thrombectomy-based IAT has advantages over thrombolytic-based IAT in terms of the reduction of groin puncture to reperfusion time and improvement of the rate of complete reperfusion.
MeSH Terms
Figure
Reference
-
1. Jansen O, von Kummer R, Forsting M, Hacke W, Sartor K. Thrombolytic therapy in acute occlusion of the intracranial internal carotid artery bifurcation. AJNR Am J Neuroradiol. 1995; 16:1977–1986.2. Hernández-Pérez M, Pérez de la Ossa N, Aleu A, Millán M, Gomis M, Dorado L, et al. Natural history of acute stroke due to occlusion of the middle cerebral artery and intracranial internal carotid artery. J Neuroimaging. 2014; 24:354–358.3. Fischer U, Mono ML, Schroth G, Jung S, Mordasini P, El-Koussy M, et al. Endovascular therapy in 201 patients with acute symptomatic occlusion of the internal carotid artery. Eur J Neurol. 2013; 20:1017–1024.4. Arnold M, Nedeltchev K, Mattle HP, Loher TJ, Stepper F, Schroth G, et al. Intra-arterial thrombolysis in 24 consecutive patients with internal carotid artery T occlusions. J Neurol Neurosurg Psychiatry. 2003; 74:739–742.5. Jahan R, Duckwiler GR, Kidwell CS, Sayre JW, Gobin YP, Villablanca JP, et al. Intraarterial thrombolysis for treatment of acute stroke: experience in 26 patients with long-term follow-up. AJNR Am J Neuroradiol. 1999; 20:1291–1299.6. Zaidat OO, Suarez JI, Santillan C, Sunshine JL, Tarr RW, Paras VH, et al. Response to intra-arterial and combined intravenous and intra-arterial thrombolytic therapy in patients with distal internal carotid artery occlusion. Stroke. 2002; 33:1821–1826.7. Lin R, Vora N, Zaidi S, Aleu A, Jankowitz B, Thomas A, et al. Mechanical approaches combined with intra-arterial pharmacological therapy are associated with higher recanalization rates than either intervention alone in revascularization of acute carotid terminus occlusion. Stroke. 2009; 40:2092–2097.8. Qureshi AI, Janjua N, Kirmani JF, Harris-Lane P, Suri MF, Zhou J, et al. Mechanical disruption of thrombus following intravenous tissue plasminogen activator for ischemic st-roke. J Neuroimaging. 2007; 17:124–130.9. Sorimachi T, Fujii Y, Tsuchiya N, Nashimoto T, Harada A, Ito Y, et al. Recanalization by mechanical embolus disruption during intra-arterial thrombolysis in the carotid territory. AJNR Am J Neuroradiol. 2004; 25:1391–1402.10. Mokin M, Kass-Hout T, Kass-Hout O, Dumont TM, Kan P, Snyder KV, et al. Intravenous thrombolysis and endovascular therapy for acute ischemic stroke with internal carotid artery occlusion: a systematic review of clinical outcomes. Stroke. 2012; 43:2362–2368.11. Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012; 380:1241–1249.12. Taschner CA, Treier M, Schumacher M, Berlis A, Weber J, Niesen W. Mechanical thrombectomy with the Penumbra recanalization device in acute ischemic stroke. J Neuroradiol. 2011; 38:47–52.13. Nogueira RG, Lutsep HL, Gupta R, Jovin TG, Albers GW, Walker GA, et al. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet. 2012; 380:1231–1240.14. Kang DH, Hwang YH, Kim YS, Park J, Kwon O, Jung C. Direct thrombus retrieval using the reperfusion catheter of the penumbra system: forced-suction thrombectomy in acute ischemic stroke. AJNR Am J Neuroradiol. 2011; 32:283–287.15. Menon BK, Puetz V, Kochar P, Demchuk AM. ASPECTS and other neuroimaging scores in the triage and prediction of outcome in acute stroke patients. Neuroimaging Clin N Am. 2011; 21:407–423. xii16. Kim JT, Park MS, Choi KH, Nam TS, Choi SM, Lee SH, et al. The CBV-ASPECT Score as a predictor of fatal stroke in a hyperacute state. Eur Neurol. 2010; 63:357–363.17. Liebeskind DS, Flint AC, Budzik RF, Xiang B, Smith WS, Duckwiler GR, et al. Carotid I's, L's and T's: collaterals shape the outcome of intracranial carotid occlusion in acute ischemic stroke. J Neurointerv Surg. 2015; 7:402–407.18. Puetz V, Dzialowski I, Hill MD, Subramaniam S, Sylaja PN, Krol A, et al. Intracranial thrombus extent predicts clinical outcome, final infarct size and hemorrhagic transformation in ischemic stroke: the clot burden score. Int J Stroke. 2008; 3:230–236.19. Zaidat OO, Yoo AJ, Khatri P, Tomsick TA, von Kummer R, Saver JL, et al. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. 2013; 44:2650–2663.20. Higashida R, Furlan A, Roberts H, Tomsick T, Connors B, Barr J, et al. Trial design and reporting standards for intraarterial cerebral thrombolysis for acute ischemic stroke. J Vasc Interv Radiol. 2003; 14(9 Pt 2):S493–S494.21. Kappelhof M, Marquering HA, Berkhemer OA, Majoie CB. Intra-arterial treatment of patients with acute ischemic stroke and internal carotid artery occlusion: a literature review. J Neurointerv Surg. 2015; 7:8–15.22. Hassan AE, Chaudhry SA, Miley JT, Khatri R, Hassan SA, Suri MF, et al. Microcatheter to recanalization (procedure time) predicts outcomes in endovascular treatment in patients with acute ischemic stroke: when do we stop? AJNR Am J Neuroradiol. 2013; 34:354–359.23. Rai AT, Jhadhav Y, Domico J, Hobbs GR. Procedural predictors of outcome in patients undergoing endovascular therapy for acute ischemic stroke. Cardiovasc Intervent Radiol. 2012; 35:1332–1339.24. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030.25. Ziegler A, Ebinger M, Fiebach JB, Audebert HJ, Leistner S. Judgment of FLAIR signal change in DWI-FLAIR mismatch determination is a challenge to clinicians. J Neurol. 2012; 259:971–973.26. Weir NU, Pexman JH, Hill MD, Buchan AM. CASES investigators. How well does ASPECTS predict the outcome of acute stroke treated with IV tPA? Neurology. 2006; 67:516–518.27. Nezu T, Koga M, Kimura K, Shiokawa Y, Nakagawara J, Furui E, et al. Pretreatment ASPECTS on DWI predicts 3-month outcome following rt-PA: SAMURAI rt-PA Registry. Neurology. 2010; 75:555–561.28. Machi P, Costalat V, Lobotesis K, Maldonado IL, Vendrell JF, Riquelme C, et al. Solitaire FR thrombectomy system: immediate results in 56 consecutive acute ischemic stroke patients. J Neurointerv Surg. 2012; 4:62–66.29. Kim DJ, Kim DI, Byun JS, Jung JY, Suh SH, Kim EY, et al. Simple microwire and microcatheter mechanical thrombolysis with adjuvant intraarterial urokinase for treatment of hyperacute ischemic stroke patients. Acta Radiol. 2008; 49:351–357.30. Todo A, Minaeian A, Sahni R, Chao KH. Incidence and outcome of procedural distal emboli using the Penumbra thrombectomy for acute stroke. J Neurointerv Surg. 2013; 5:135–138.31. King S, Khatri P, Carrozella J, Spilker J, Broderick J, Hill M, et al. Anterior cerebral artery emboli in combined intravenous and intra-arterial rtPA treatment of acute ischemic stroke in the IMS I and II trials. AJNR Am J Neuroradiol. 2007; 28:1890–1894.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Aspiration Clot Removal by Mannual Compression of Common Carotid Artery for Acute Internal Carotid Occlusion: a Case Report
- Urgent Recanalization Using Stents for Acute Internal Carotid Artery Occlusion in Progressive Stroke Patients with Contralateral Chronic Carotid Occlusion
- Rescue Treatment with Intra-arterial Tirofiban Infusion and Emergent Carotid Stenting
- Symptomatic Bilateral Carotid Artery Occlusion: An Uncommon Pattern of Carotid Pathology
- Differentiating Carotid Terminus Occlusions into Two Distinct Populations Based on Willisian Collateral Status