Korean J Urol.
2012 Sep;53(9):619-624. 10.4111/kju.2012.53.9.619.
Roles of Urology as Assessed by an Analysis of Inpatients Referred to Urology
- Affiliations
-
- 1Department of Urology, Chosun University School of Medicine, Gwangju, Korea. uro2097@gmail.com
- KMID: 2061700
- DOI: http://doi.org/10.4111/kju.2012.53.9.619
Abstract
- PURPOSE
The purpose of this study was to identify the necessity for professional urology treatment and the roles of urology in the treatment of inpatients referred to the urology department.
MATERIALS AND METHODS
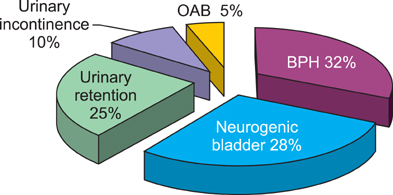
The subjects were patients referred to the department of urology among the inpatients of Chosun University Hospital from January 1, 2009, to December 31, 2011. The patients' sex and age, the referring department, and the disease group were extracted from the patients' medical records. Disease groups were classified as urination disorder, infection, tumor, calculus, trauma, pediatrics, andrology, and others. The urination disorder group was classified into the subcategories of neurogenic bladder, benign prostatic hypertrophy, urinary retention, urinary incontinence, and overactive bladder.
RESULTS
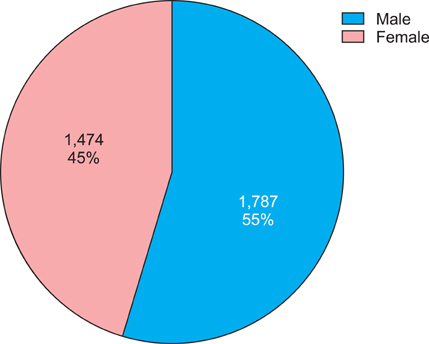
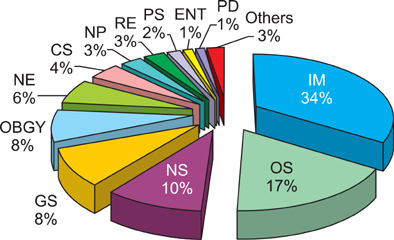
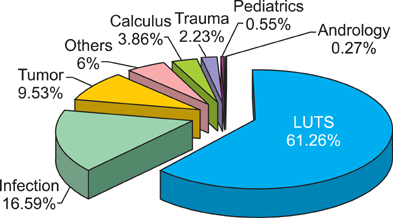
The total number of referrals was 3,261, and males made up 54.79%. In the age distribution, 2,321 patients (71.17%) were over 60 years of age and the largest population group was patients in their 70s (32.72%). According to the department referring the patients, internal medicine (34.06%) and orthopedic surgery (16.83%) made up a high percentage. Concerning the disease group, urination disorder was the highest, being 61.26%. In the subclassification of the urination disorder group, benign prostatic hypertrophy was the highest category at 32.23%.
CONCLUSIONS
In this urology cooperative behavior analysis of our hospital over 3 years, a high percentage of older patients over 60 years of age and a high percentage of urination disorders were found. Urination disorder-related diseases in persons of advanced age are expected to increase as Korea becomes an aged society, and doctors in other departments should be aware that professional treatment and management by a urologist is needed for the treatment of these disorders.
MeSH Terms
Figure
Reference
-
1. Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998. 97:1837–1847.2. 27th Bethesda Conference. Matching the Intensity of Risk Factor Management with the Hazard for Coronary Disease Events. September 14-15, 1995. J Am Coll Cardiol. 1996. 27:957–1047.3. Boon TA, Van Venrooij GE, Eckhardt MD. Effect of diabetes mellitus on lower urinary tract symptoms and dysfunction in patients with benign prostatic hyperplasia. Curr Urol Rep. 2001. 2:297–301.4. Michel MC, Heemann U, Schumacher H, Mehlburger L, Goepel M. Association of hypertension with symptoms of benign prostatic hyperplasia. J Urol. 2004. 172(4 Pt 1):1390–1393.5. Hammarsten J, Högstedt B, Holthuis N, Mellström D. Components of the metabolic syndrome-risk factors for the development of benign prostatic hyperplasia. Prostate Cancer Prostatic Dis. 1998. 1:157–162.6. Health Insurance Review & Assessment Service [Internet]. c2011. cited 2012 Feb 23. Seoul: Health Insurance Review & Assessment Service;Available from: http://www.hira.or.kr/main.do.7. Shin CW, Kim SD, Cho WY. The prevalence and management of urinary incontinence in elderly patients at sanatorium in Busan area. Korean J Urol. 2009. 50:450–456.8. Korea National Statistical Office. Population projections for Korea. 2006. Seoul: Korean National Statistical Office.9. Korean Ministry of Health and Welfare. Yearbook on health and welfare statistics. 2007. 53rd ed. Seoul: Korean Ministry of Health and Welfare.10. Lee YS, Lee KS, Jung JH, Han DH, Oh SJ, Seo JT, et al. Prevalence of overactive bladder, urinary incontinence, and lower urinary tract symptoms: results of Korean EPIC study. World J Urol. 2011. 29:185–190.11. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984. 132:474–479.12. Garraway WM, Collins GN, Lee RJ. High prevalence of benign prostatic hypertrophy in the community. Lancet. 1991. 338:469–471.13. Yoo TK, Cho HJ. Benign prostatic hyperplasia: from bench to clinic. Korean J Urol. 2012. 53:139–148.14. Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988. 37:1595–1607.15. Hammarsten J, Högstedt B. Hyperinsulinaemia as a risk factor for developing benign prostatic hyperplasia. Eur Urol. 2001. 39:151–158.16. Matsuda T, Abe H, Suda K. Relation between benign prostatic hyperplasia and obesity and estrogen. Rinsho Byori. 2004. 52:291–294.17. Hoepelman AI, Meiland R, Geerlings SE. Pathogenesis and management of bacterial urinary tract infections in adult patients with diabetes mellitus. Int J Antimicrob Agents. 2003. 22:Suppl 2. 35–43.18. Giugliano F, Esposito K, Di Palo C, Ciotola M, Giugliano G, Marfella R, et al. Erectile dysfunction associates with endothelial dysfunction and raised proinflammatory cytokine levels in obese men. J Endocrinol Invest. 2004. 27:665–669.19. Neil M. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Geriatric incontinence and voiding dysfunction. Campbell-Walsh Urology. 2011. 10th edition. Philadelphia: Saunders;2206–2207.20. Wein AJ. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Lower urinary tract dysfunction in neurologic injury and disease. Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders;2040–2041.21. Petros JG, Rimm EB, Robillard RJ. Factors influencing urinary tract retention after elective open cholecystectomy. Surg Gynecol Obstet. 1992. 174:497–500.22. Stallard S, Prescott S. Postoperative urinary retention in general surgical patients. Br J Surg. 1988. 75:1141–1143.23. Kwon MI, Kim KM, Kim KW, Kim BK, Kim SY, Kim SD, et al. Anesthesiology. 2005. 3rd ed. Seoul: Ryomoongak.24. Hozack WJ, Carpiniello V, Booth RE Jr. The effect of early bladder catheterization on the incidence of urinary complications after total joint replacement. Clin Orthop Relat Res. 1988. (231):79–82.25. Wren KR, Wren TL. Postsurgical urinary retention. Urol Nurs. 1996. 16:45–47.26. Oh SJ, Park WH, Park CH, Paick JS, Seo JT, Lee YS, et al. Prevalence of urinary incontinence and incontinence-related quality of life in Korean women: a Population-based Study. J Korean Continence Soc. 2003. 7:73–80.27. Cho YH. Introduction to urinary tract infections. Korean J Urol. 2006. 47:559–567.28. Naber KG, Bishop MC, Bjerklund-Johansen TE, Botto H, Cek M, Grabe M, et al. European Association of Urology. The management of urinary and male genital tract infections. European Association of Urology Guidelines. 2006. Arnhem: Drukkerij Gelderland;1–126.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Statistical Observation on Patients with Pediatric Urological Disease.
- Clinical Observation on Patients with Pediatric Urological Disease
- Statistical Observation on In-patient(1967~1970)
- A Clinical Observation on the Pediatric Diseases in Urology
- A Recent 10 Year's Clinical Observation on Disease of Pediatric Urology