Korean J Urol.
2013 May;54(5):339-344. 10.4111/kju.2013.54.5.339.
Effects of Mirodenafil, a Phosphodiesterase-5 Inhibitor, on Female Rat Bladder in a Partial Bladder Outlet Obstruction Model: Physiological and Immunohistochemical Aspects
- Affiliations
-
- 1Department of Urology, Eulji General Hospital, Seoul, Korea.
- 2Department of Pathology, Eulji General Hospital, Seoul, Korea.
- 3Department of Urology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. kwang@plaza.snu.ac.kr
- KMID: 2061517
- DOI: http://doi.org/10.4111/kju.2013.54.5.339
Abstract
- PURPOSE
We investigated the effects of mirodenafil, a phosphodiesterase-5 inhibitor developed in South Korea, on the female rat bladder in a partial bladder outlet obstruction (BOO) model.
MATERIALS AND METHODS
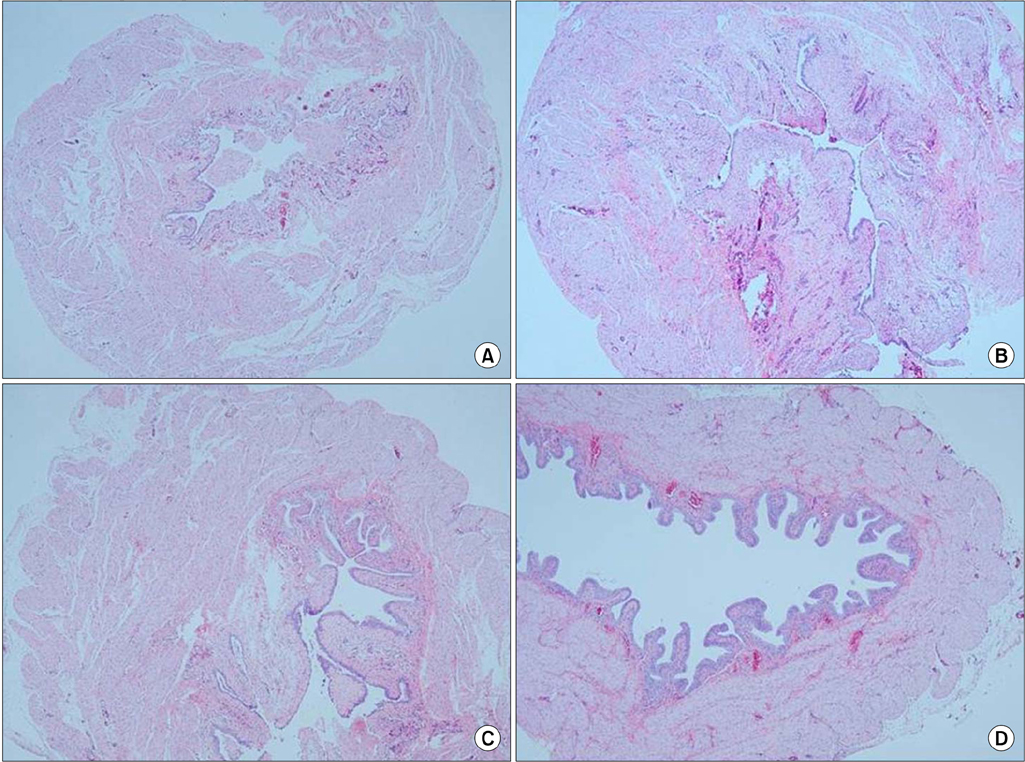
Thirty-six female Sprague-Dawley rats were divided into four groups: the control group, BOO without medication group, BOO with mirodenafil 1 mg/kg group, and BOO with mirodenafil 4 mg/kg group. Mirodenafil was administered orally for 2 weeks after the induction of BOO. Two weeks after BOO, the rats in each group underwent cystometry under urethane anesthesia. After cystometry, the bladder was excised to perform immunohistochemical staining for connexin 43.
RESULTS
The three BOO groups showed significant increases in mean bladder weight compared with the control group. Baseline pressure, threshold pressure, and maximum contraction pressure were not significantly different between the four groups. Although the contraction interval was decreased in all BOO groups compared with the control group, it was prolonged in the two groups treated with mirodenafil compared with the untreated BOO group. In the immunohistochemical examination, connexin 43 staining intensity in the lamina propria increased in the three BOO groups compared with the control group. The two groups treated with mirodenafil, however, showed decreased connexin 43 staining compared with the untreated BOO group.
CONCLUSIONS
Mirodenafil may increase the contraction intervals of female rat bladders in a partial BOO model. Decreasing bladder overactivity by mirodenafil may be related to intracellular communication mechanisms involving connexin 43.
Keyword
MeSH Terms
-
Anesthesia
Animals
Connexin 43
Contracts
Cyclic Nucleotide Phosphodiesterases, Type 5
Female
Humans
Mucous Membrane
Phosphodiesterase Inhibitors
Pyrimidinones
Rats
Rats, Sprague-Dawley
Republic of Korea
Sulfonamides
Urethane
Urinary Bladder
Urinary Bladder Neck Obstruction
Urinary Bladder, Overactive
Connexin 43
Cyclic Nucleotide Phosphodiesterases, Type 5
Phosphodiesterase Inhibitors
Pyrimidinones
Sulfonamides
Urethane
Figure
Reference
-
1. Liu L, Zheng S, Han P, Wei Q. Phosphodiesterase-5 inhibitors for lower urinary tract symptoms secondary to benign prostatic hyperplasia: a systematic review and meta-analysis. Urology. 2011. 77:123–129.2. Gacci M, Vittori G, Tosi N, Siena G, Rossetti MA, Lapini A, et al. A randomized, placebo-controlled study to assess safety and efficacy of vardenafil 10 mg and tamsulosin 0.4 mg vs. tamsulosin 0.4 mg alone in the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Sex Med. 2012. 9:1624–1633.3. Qiu Y, Kraft P, Craig EC, Liu X, Haynes-Johnson D. Identification and functional study of phosphodiesterases in rat urinary bladder. Urol Res. 2001. 29:388–392.4. Haferkamp A, Mundhenk J, Bastian PJ, Reitz A, Dorsam J, Pannek J, et al. Increased expression of connexin 43 in the overactive neurogenic detrusor. Eur Urol. 2004. 46:799–805.5. Kim JC, Kim DB, Seo SI, Park YH, Hwang TK. Effects of connexin expression on unstable bladder after relief of bladder outlet obstruction in rat. Korean J Urol. 2003. 44:585–591.6. Mattiasson A, Uvelius B. Changes in contractile properties in hypertrophic rat urinary bladder. J Urol. 1982. 128:1340–1342.7. Ikeda Y, Fry C, Hayashi F, Stolz D, Griffiths D, Kanai A. Role of gap junctions in spontaneous activity of the rat bladder. Am J Physiol Renal Physiol. 2007. 293:F1018–F1025.8. Miyazato M, Sugaya K, Nishijima S, Kadekawa K, Machida N, Oshiro Y, et al. Changes of bladder activity and connexin 43-derived gap junctions after partial bladder-outlet obstruction in rats. Int Urol Nephrol. 2009. 41:815–821.9. Kim HS, Kim JC, Hwang TK. Effect of ACE inhibitor on connexin expression after bladder outlet obstruction in rats. Korean J Urol. 2005. 46:1205–1212.10. Sui GP, Rothery S, Dupont E, Fry CH, Severs NJ. Gap junctions and connexin expression in human suburothelial interstitial cells. BJU Int. 2002. 90:118–129.11. Kanai A, Roppolo J, Ikeda Y, Zabbarova I, Tai C, Birder L, et al. Origin of spontaneous activity in neonatal and adult rat bladders and its enhancement by stretch and muscarinic agonists. Am J Physiol Renal Physiol. 2007. 292:F1065–F1072.12. Nishiguchi J, Kwon DD, Kaiho Y, Chancellor MB, Kumon H, Snyder PB, et al. Suppression of detrusor overactivity in rats with bladder outlet obstruction by a type 4 phosphodiesterase inhibitor. BJU Int. 2007. 99:680–686.13. Tinel H, Stelte-Ludwig B, Hutter J, Sandner P. Pre-clinical evidence for the use of phosphodiesterase-5 inhibitors for treating benign prostatic hyperplasia and lower urinary tract symptoms. BJU Int. 2006. 98:1259–1263.14. McVary KT, Roehrborn CG, Kaminetsky JC, Auerbach SM, Wachs B, Young JM, et al. Tadalafil relieves lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol. 2007. 177:1401–1407.15. Gacci M, Del Popolo G, Macchiarella A, Celso M, Vittori G, Lapini A, et al. Vardenafil improves urodynamic parameters in men with spinal cord injury: results from a single dose, pilot study. J Urol. 2007. 178:2040–2043.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role of Peripheral and Spinal alpha1-adrenoceptor in Bladder Overactivity Induced by Partial Bladder Outlet Obstruction in Rat
- Effect of Bladder Outlet Obstruction on Blood Flow and Tissue Collagen in Rat Bladder
- Mirodenafil Prevents Bladder Dysfunction Induced by Chronic Bladder Ischemia in Rats
- Ultrastructural Changes of Detrusor Muscle by Partial Obstruction of the Bladder Outlet in the Rat
- Changes in Detrusor and Urinary Growth Factors According to the Bladder Function after Partial Bladder Outlet Obstruction in Rat