Electrolyte Blood Press.
2008 Jun;6(1):15-21. 10.5049/EBP.2008.6.1.15.
Relationship between Serum N-Terminal Pro-Brain Natriuretic Peptide Level and Left Ventricular Dysfunction and Extracellular Water in Continuous Ambulatory Peritoneal Dialysis Patients
- Affiliations
-
- 1Division of Nephrology, Department of Internal Medicine, Chosun University College of Medicine, Gwangju, Korea. hyunkim@chosun.ac.kr
- KMID: 2052301
- DOI: http://doi.org/10.5049/EBP.2008.6.1.15
Abstract
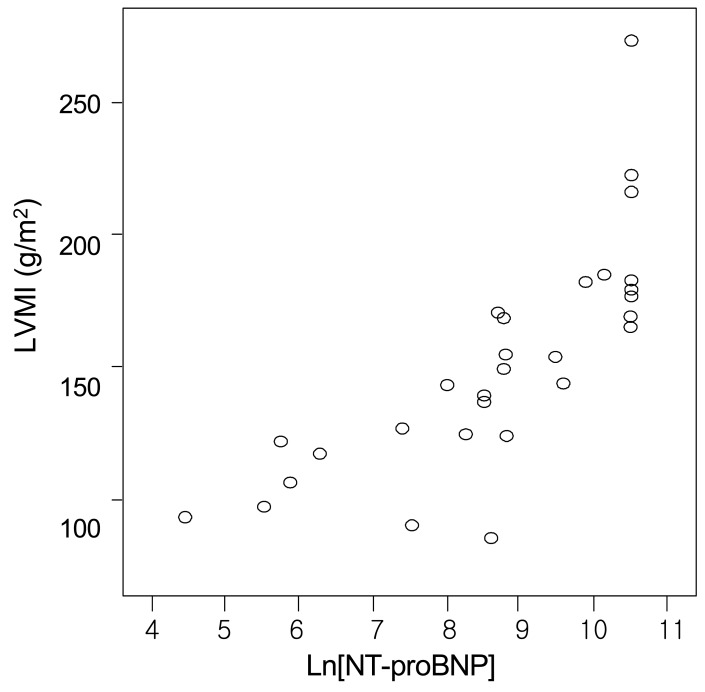
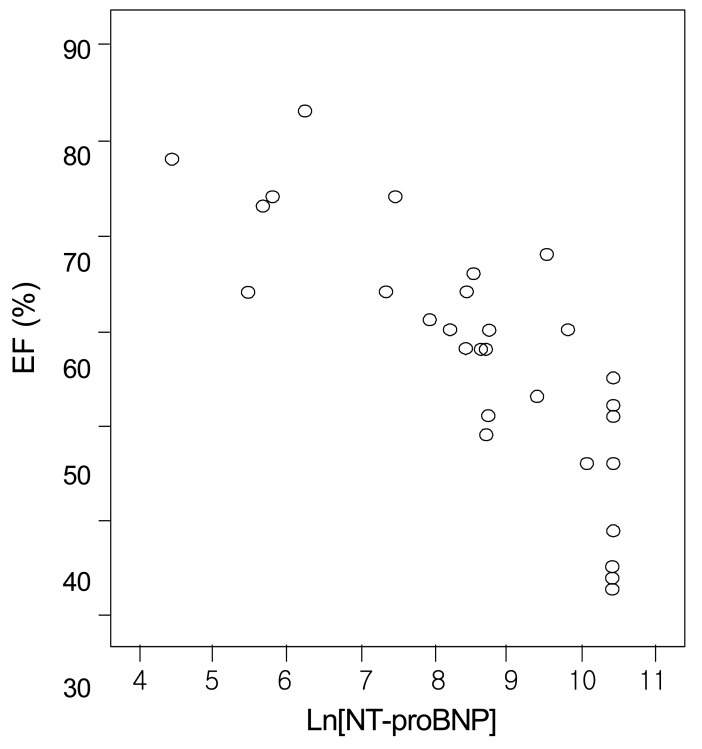
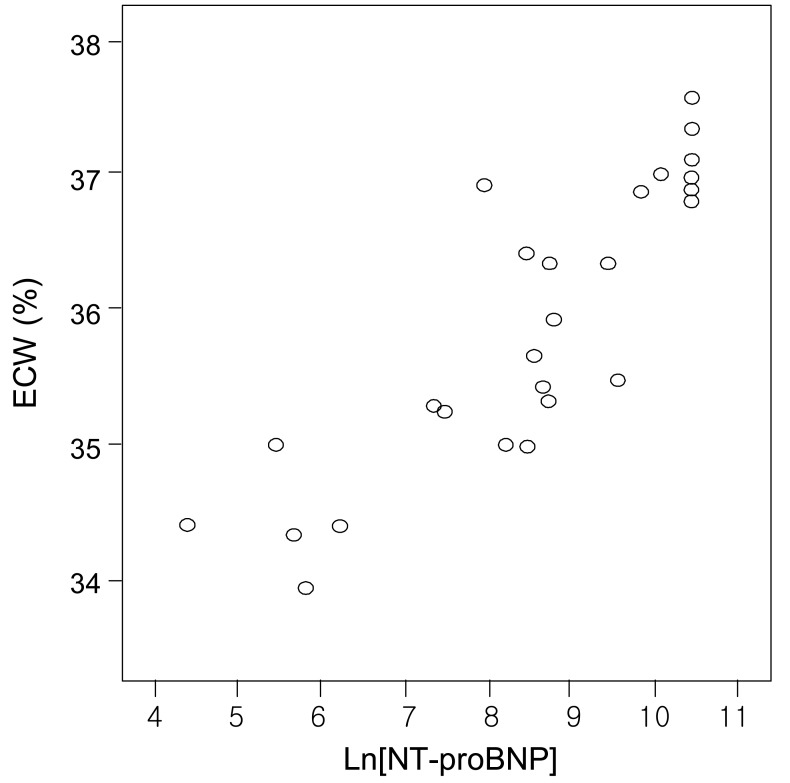
- This study inquired the relationship between serum N-terminal pro-brain natriuretic peptide (NT-proBNP) levels and left ventricular (LV) dysfunction and extracellular water in continuous ambulatory peritoneal dialysis (CAPD) patients. We conducted a cross-sectional study of 30 CAPD patients. Each patient was admitted to the department of internal medicine, Chosun University Hospital between February and October, 2006. Echocardiography was performed using HDI 5000, allowing M-mode, two-dimensional measurement. A multifrequency bioimpedance analyzer was used; extracellular water was calculated as a percentage of total body water and was understood as the index of volume load of CAPD patients. The mean age was 47+/-12 years. Underlying causes of renal failure were 14 with diabetes mellitus, 7 with hypertension, and 9 with chronic glomerulonephritis. The mean serum NT-proBNP level was 14236.56 (83-35,000) pg/mL. LV mass index and LV ejection fraction were 151.67+/-42.5 g/m2 and 57.48+/-12.9%, respectively. The mean extracellular water was 35.97+/-1.04%. Serum NT-proBNP levels correlated positively with LV mass index (r=0.768, p=0.01) and extracellular water (r=0.866, p=0.01) and negatively with LV ejection fraction (r= -0.808, p=0.01). Serum NT-proBNP levels significantly correlated with LV mass index, LV ejection fraction, and extracellular water. Therefore, serum NT-proBNP levels can be a clinical predictive marker for LV hypertrophy, LV dysfunction, and volume status in CAPD patients.
MeSH Terms
-
Body Water
Cross-Sectional Studies
Diabetes Mellitus
Echocardiography
Extracellular Fluid
Glomerulonephritis
Humans
Hypertension
Hypertrophy
Internal Medicine
Natriuretic Peptide, Brain
Peptide Fragments
Peritoneal Dialysis, Continuous Ambulatory
Renal Insufficiency
Ventricular Dysfunction, Left
Extracellular Fluid
Natriuretic Peptide, Brain
Peptide Fragments
Figure
Cited by 1 articles
-
Comparison of Blood Pressure Control and Left Ventricular Hypertrophy in Patients on Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD)
Jong Soon Jang, Soon Kil Kwon, Hye-Young Kim
Electrolyte Blood Press. 2011;9(1):16-22. doi: 10.5049/EBP.2011.9.1.16.
Reference
-
1. Culleton BF, Larson MG, Wilson PW, Evans JC, Parfrey PS, Levy D. Cardiovascular disease and mortality in a community-based cohort with mild renal insufficiency. Kidney Int. 1999; 56:2214–2219. PMID: 10594797.
Article2. Foley RN, Parfrey PS, Sarnak MJ. Epidemiology of cardiovascular disease in chronic renal disease. J Am Soc Nephrol. 1998; 9:S16–S23. PMID: 11443763.3. K/DOQI Workgroup. K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patiets. Am J Kidney Dis. 2005; 45(Suppl 3):S1–S153.4. Murdoch DR, Byrne J, Morton JJ, McDonagh TA, Robb SD, Clements S, et al. Brain natriuretic peptide is stable in whole blood and can be measured using a simple rapid assay: implications for clinical practice. Heart. 1997; 78:594–597. PMID: 9470878.
Article5. Bay M, Kirk V, Parner J, Hassager C, Nielsen H, Krogsgaard K, et al. NT-proBNP: a new diagnostic screening tool to differentiate between patients with normal and reduced left ventricular systolic function. Heart. 2003; 89:150–154. PMID: 12527664.
Article6. Kwon SH, On YK, Han DH, Lee SC, Jo YH, Lee NH, et al. Usefulness of B-type Natriuretic Peptide in Congestive Heart Failure. Korean Circ J. 2003; 33:695–700.
Article7. DeFilippi CR, Fink JC, Nass CM, Chen H, Christenson R. N-terminal pro-B-type natriuretic peptide for predicting coronary disease and left ventricular hypertrophy in asymptomatic CKD not requiring dialysis. Am J Kidney Dis. 2005; 46:35–44. PMID: 15983955.
Article8. Choi SY, Kim JA, Lee JE, Do YS, Jang EH, Bae HJ, et al. Plasma Levels of N-terminal pro-brain Natriuretic Peptide (NT-proBNP) and Left Ventricular Function in Patients with Chronic Renal Failure. Korean J Nephrol. 2006; 25:413–421.9. Zoccali C, Mallamaci F, Benedetto FA, Tripepi G, Parlongo S, Cataliotti A, et al. Cardiac natriuretic peptides are related to left ventricular mass and function and predict mortality in dialysis patients. J Am Soc Nephrol. 2001; 12:1508–1515. PMID: 11423580.
Article10. Ganau A, Devereux RB, Roman MJ, de Simone G, Pickering TG, Saba PS, et al. Patterns of left ventricular hypertrophy and geometric remodeling in essential hypertension. J Am Coll Cardiol. 1992; 19:1550–1558. PMID: 1534335.
Article11. Snel YE, Brummer RJ, Doerga ME, Zelissen PM, Koppeschaar HP. Validation of extracellular water determination by bioelectrical impedance analysis in growth hormone-deficient adults. Ann Nutr Metab. 1995; 39:242–250. PMID: 8546441.
Article12. Levy D, Savage DD, Garrison RJ, Anderson KM, Kannel WB, Castelli WP. Echocardiographic criteria for left ventricular hypertrophy: the Framingham Heart Study. Am J Cardiol. 1987; 59:956–960. PMID: 2952002.
Article13. Stoddard MF, Pearson AC, Kern MJ, Ratcliff J, Mrosek DG, Labovitz AJ. Influence of alteration in preload on the pattern of left ventricular diastolic filling as assessed by Doppler echocardiography in humans. Circulation. 1989; 79:1226–1236. PMID: 2498005.
Article14. Brun P, Tribouilloy C, Duval AM, Iserin L, Meguira A, Pelle G, et al. Left ventricular flow propagation during early filling is related to wall relaxation: a color M-mode Doppler analysis. J Am Coll Cardiol. 1992; 20:420–432. PMID: 1634681.
Article15. Naganuma T, Sugimura K, Wada S, Yasumoto R, Sugimura T, Masuda C, et al. The prognostic role of brain natriuretic peptides in hemodialysis patients. Am J Nephrol. 2002; 22:437–444. PMID: 12381941.
Article16. Nishikimi T, Futoo Y, Tamano K, Takahashi M, Suzuki T, Minami J, et al. Plasma brain natriuretic peptide levels in chronic hemodialysis patients: influence of coronary artery disease. Am J Kidney Dis. 2001; 37:1201–1208. PMID: 11382689.
Article17. Fagugli RM, Palumbo B, Ricciardi D, Pasini P, Santirosi P, Vecchi L, et al. Association between brain natriuretic peptide and extracellular water in hemodialysis patients. Nephron Clin Pract. 2003; 95:C60–C66. PMID: 14610331.
Article18. Su X, Brower G, Janicki JS, Chen YF, Oparil S, Dell'Italia LJ. Differential expression of natriuretic peptides and their receptors in volume overload cardiac hypertrophy in the rat. J Mol Cell Cardiol. 1999; 31:1927–1936. PMID: 10525429.
Article19. Dastoor H, Bernieh B, Boobes Y, Abouchacra S, Eltayeb E, Elhuda MN, et al. Plasma BNP in patients on maintenance haemodialysis: a guide to management? J Hypertens. 2005; 23:23–28. PMID: 15643118.20. Lee JA, Kim DH, Yoo SJ, Oh DJ, Yu SH, Kang ET. Association between serum n-terminal pro-brain natriuretic peptide concentration and left ventricular dysfunction and extracellular water in continuous ambulatory peritoneal dialysis patients. Perit Dial Int. 2006; 26:360–365. PMID: 16722030.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Association Between Left Ventricular Hypertrophy and Biomarkers in Patients on Continuous Ambulatory Peritoneal Dialysis
- Changes in extracellular water and left ventricular mass in peritoneal dialysis patients
- Comparison of Blood Pressure Control and Left Ventricular Hypertrophy in Patients on Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD)
- Correlation of N-Terminal Pro-Brain Type Natriuretic Peptide Level and Echocardiographic Parameters
- Correlation between N-Terminal Pro-Brain Natriuretic Peptide and Doppler Echocardiographic Parameters of Left Ventricular Filling Pressure in Atrial Fibrillation