Neurointervention.
2013 Feb;8(1):29-33. 10.5469/neuroint.2013.8.1.29.
Trans-sphenoidal Approach to the Supraclinoid Internal Carotid Artery for Endovascular Access in a Cadaver
- Affiliations
-
- 1Department of Neurological Surgery, Rush University Medical Center, Chicago, IL, USA. andrew_johnson@rush.edu
- 2Rush Medical College, Chicago, IL, USA.
- 3Department of Anatomy, Rush University Medical Center, Chicago, IL, USA.
- KMID: 2052078
- DOI: http://doi.org/10.5469/neuroint.2013.8.1.29
Abstract
- PURPOSE
Sometimes, intracranial pathology in the distal vasculature cannot be accessed by standard endovascular techniques because of occlusion or insurmountable tortuosity of theinternal carotid artery (ICA). A trans-sphenoidal surgical approach can follow a similar trajectory to the course of the supraclinoid ICA. This study evaluates the feasibility of a trans-sphenoidal approach to the supraclinoid ICA for endovascular access.
MATERIALS AND METHODS
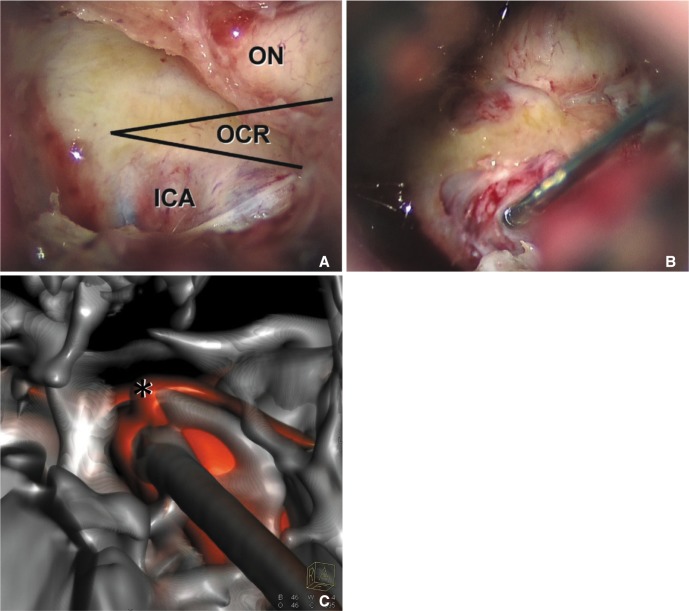
In a fresh cadaver head, the sphenoid sinus was dissected through a trans-sphenoidal route. Bone over the carotid prominence was removed to expose the ICA. The artery was catheterized using the Seldinger technique, and three-dimensional digital subtraction angiography was performed to evaluate the procedure.
RESULTS
The catheter was successfully inserted into the supraclinoid ICA via the trans-sphenoidal route. Three-dimensional radiographic reconstruction confirmed placement of the catheter and the trajectory of the sheath into the supraclinoid ICA.
CONCLUSION
While the trans-sphenoidal route has innumerable disadvantages over the standard endovascular access techniques, this route could be considered when other treatment options are too risky or impractical.
MeSH Terms
Figure
Reference
-
1. Halbach VV, Higashida RT, Hieshima GB, Hardin CW. Direct puncture of the proximally occluded internal carotid artery for treatment of carotid cavernous fistulas. AJNR Am J Neuroradiol. 1989; 10:151–154. PMID: 2492715.2. Tsai YH, Weng HH, Chen YL, Wu YM, Wong HF. Treatment of recurrent carotid cavernous fistula by direct puncture of a previously trapped internal carotid artery. J Vasc Interv Radiol. 2010; 21:738–740. PMID: 20304678.
Article4. Kono Y, Prevedello DM, Snyderman CH, Gardner PA, Kassam AB, Carrau RL, et al. One thousand endoscopic skull base surgical procedures demystifying the infection potential: incidence and description of postoperative meningitis and brain abscesses. Infect Control Hosp Epidemiol. 2011; 32:77–83. PMID: 21121816.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Supraclinoid Internal Carotid Artery Fenestration Harboring an Unruptured Aneurysm and Another Remote Ruptured Aneurysm: Case Report and Review of the Literature
- Endovascular Treatment with a Stent-Graft for Internal Carotid Artery Laceration during Trans Sphenoidal Surgery: A Case Report
- Is the retrograde access for endovascular treatment of a traumatic carotid cavernous fistula associated with dissection of the ipsilateral carotid possible?
- Endovascular Treatment of Cavernous Sinus Dural Arteriovenous Fistula via Radial Artery and Median Cubital Vein
- Microsurgical Anatomy of the Supraclinoid Internal Carotid Artery