Ann Surg Treat Res.
2015 Jul;89(1):23-29. 10.4174/astr.2015.89.1.23.
Oncologic outcomes in rectal cancer with close distal resection margins: a retrospective analysis
- Affiliations
-
- 1Department of Surgery, Ewha Womans University School of Medicine, Seoul, Korea. eastgate@ewha.ac.kr
- KMID: 2047710
- DOI: http://doi.org/10.4174/astr.2015.89.1.23
Abstract
- PURPOSE
The assurance of a negative resection margin is significant in rectal cancer as it indicates a reduced risk of local recurrence; thus, sufficient length of the resection margin is strongly required. The purpose of this study was to analyze the relationship between the length of the distal resection margin (DRM) and local recurrence or survival rate and to evaluate the possibility of performing sphincter-conserving surgery.
METHODS
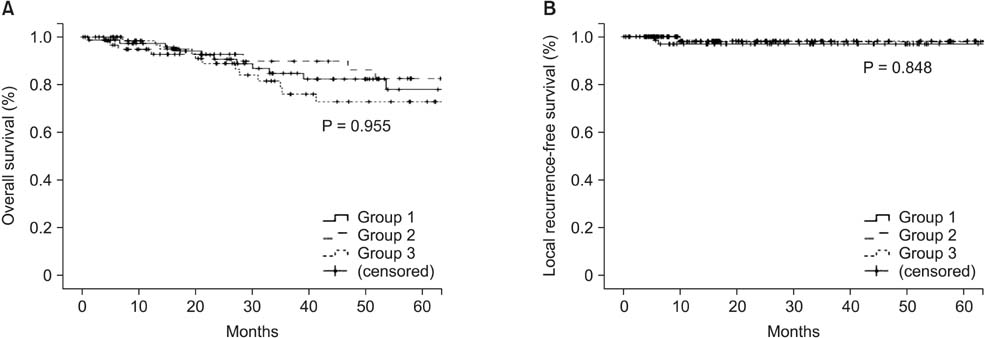
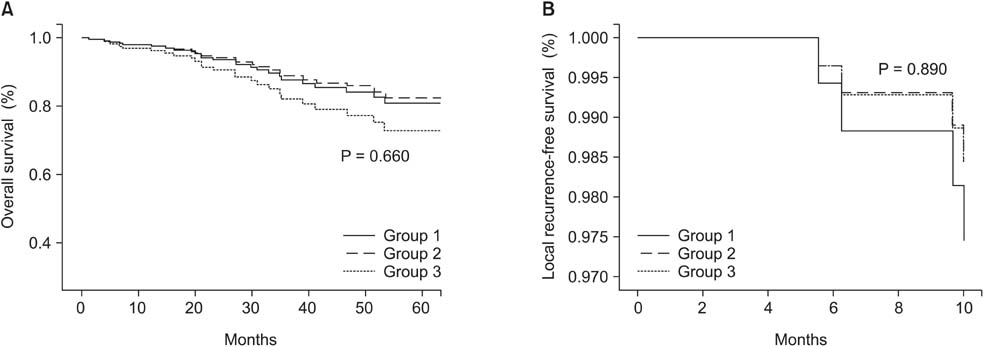
The medical records of 218 rectal cancer patients were analyzed. Patients were classified into three groups according to the length of the DRM as follows: group 1, DRM < 1 cm; group 2, 1 cm < or = DRM < or = 2 cm; and group 3, DRM > 2 cm.
RESULTS
Of 218 patients enrolled, 81 were in group 1, 66 in group 2, and 71 in group 3. The 5-year survival rates were 78.2%, 78.2%, and 76.8% for groups 1, 2, and 3, respectively, and there were no statistically significant differences in survival (P = 0.913). Local recurrence was found in 2 patients in group 1, 1 patient in group 2, and 1 patient in group 3; there were no statistically significant differences in local recurrence (P = 0.908).
CONCLUSION
A DRM of < 1 cm did not impair the oncologic outcomes of rectal cancer patients. Our results indicated that surgeons should keep in mind to consider the option of sphincter-conserving surgery with adjuvant chemoradiotherapy even in very low rectal cancer.
MeSH Terms
Figure
Reference
-
1. Nelson H, Petrelli N, Carlin A, Couture J, Fleshman J, Guillem J, et al. Guidelines 2000 for colon and rectal cancer surgery. J Natl Cancer Inst. 2001; 93:583–596.2. Lim SB, Kim JC. Surgical issues in locally advanced rectal cancer treated by preoperative chemoradiotherapy. J Korean Surg Soc. 2013; 84:1–8.3. Scott N, Jackson P, al-Jaberi T, Dixon MF, Quirke P, Finan PJ. Total mesorectal excision and local recurrence: a study of tumour spread in the mesorectum distal to rectal cancer. Br J Surg. 1995; 82:1031–1033.4. Cecil TD, Sexton R, Moran BJ, Heald RJ. Total mesorectal excision results in low local recurrence rates in lymph node-positive rectal cancer. Dis Colon Rectum. 2004; 47:1145–1149.5. Van Cutsem E, Dicato M, Haustermans K, Arber N, Bosset JF, Cunningham D, et al. The diagnosis and management of rectal cancer: expert discussion and recommendations derived from the 9th World Congress on Gastrointestinal Cancer, Barcelona, 2007. Ann Oncol. 2008; 19:Suppl 6. vi1–vi8.6. Bujko K, Rutkowski A, Chang GJ, Michalski W, Chmielik E, Kusnierz J. Is the 1-cm rule of distal bowel resection margin in rectal cancer based on clinical evidence? A systematic review. Ann Surg Oncol. 2012; 19:801–808.7. Kiran RP, Lian L, Lavery IC. Does a subcentimeter distal resection margin adversely influence oncologic outcomes in patients with rectal cancer undergoing restorative proctectomy? Dis Colon Rectum. 2011; 54:157–163.8. Nash GM, Weiss A, Dasgupta R, Gonen M, Guillem JG, Wong WD. Close distal margin and rectal cancer recurrence after sphincter-preserving rectal resection. Dis Colon Rectum. 2010; 53:1365–1373.9. Vernava AM 3rd, Moran M, Rothenberger DA, Wong WD. A prospective evaluation of distal margins in carcinoma of the rectum. Surg Gynecol Obstet. 1992; 175:333–336.10. Karanjia ND, Schache DJ, North WR, Heald RJ. 'Close shave' in anterior resection. Br J Surg. 1990; 77:510–512.11. Kuvshinoff B, Maghfoor I, Miedema B, Bryer M, Westgate S, Wilkes J, et al. Distal margin requirements after preoperative chemoradiotherapy for distal rectal carcinomas: are < or = 1 cm distal margins sufficient? Ann Surg Oncol. 2001; 8:163–169.12. Andreola S, Leo E, Belli F, Bonfanti G, Sirizzotti G, Greco P, et al. Adenocarcinoma of the lower third of the rectum surgically treated with a <10-MM distal clearance: preliminary results in 35 N0 patients. Ann Surg Oncol. 2001; 8:611–615.13. Huh JW, Jung EJ, Park YA, Lee KY, Sohn SK. Sphincter-preserving operations following preoperative chemoradiation: an alternative to abdominoperineal resection for lower rectal cancer? World J Surg. 2008; 32:1116–1123.14. Rutkowski A, Bujko K, Nowacki MP, Chmielik E, Nasierowska-Guttmejer A, Wojnar A, et al. Distal bowel surgical margin shorter than 1 cm after preoperative radiation for rectal cancer: is it safe? Ann Surg Oncol. 2008; 15:3124–3131.15. Pricolo VE, Abodeely A, Resnick M. Distal margins in radical resections for rectal cancer after chemoradiation therapy: how short is long enough? Dig Surg. 2010; 27:185–189.16. Williams NS, Dixon MF, Johnston D. Reappraisal of the 5 centimetre rule of distal excision for carcinoma of the rectum: a study of distal intramural spread and of patients' survival. Br J Surg. 1983; 70:150–154.17. Madsen PM, Christiansen J. Distal intramural spread of rectal carcinomas. Dis Colon Rectum. 1986; 29:279–282.18. Shirouzu K, Isomoto H, Kakegawa T. Distal spread of rectal cancer and optimal distal margin of resection for sphincter-preserving surgery. Cancer. 1995; 76:388–392.19. Mezhir JJ, Smith KD, Fichera A, Hart J, Posner MC, Hurst RD. Presence of distal intramural spread after preoperative combined-modality therapy for adenocarcinoma of the rectum: what is now the appropriate distal resection margin? Surgery. 2005; 138:658–663.20. Kwok SP, Lau WY, Leung KL, Liew CT, Li AK. Prospective analysis of the distal margin of clearance in anterior resection for rectal carcinoma. Br J Surg. 1996; 83:969–972.21. Chmielik E, Bujko K, Nasierowska-Guttmejer A, Nowacki MP, Kepka L, Sopylo R, et al. Distal intramural spread of rectal cancer after preoperative radiotherapy: the results of a multicenter randomized clinical study. Int J Radiat Oncol Biol Phys. 2006; 65:182–188.22. Ross L, Abild-Nielsen AG, Thomsen BL, Karlsen RV, Boesen EH, Johansen C. Quality of life of Danish colorectal cancer patients with and without a stoma. Support Care Cancer. 2007; 15:505–513.23. Gervaz P, Bucher P, Konrad B, Morel P, Beyeler S, Lataillade L, et al. A Prospective longitudinal evaluation of quality of life after abdominoperineal resection. J Surg Oncol. 2008; 97:14–19.24. Tsunoda A, Tsunoda Y, Narita K, Watanabe M, Nakao K, Kusano M. Quality of life after low anterior resection and temporary loop ileostomy. Dis Colon Rectum. 2008; 51:218–222.25. Siassi M, Hohenberger W, Losel F, Weiss M. Quality of life and patient's expectations after closure of a temporary stoma. Int J Colorectal Dis. 2008; 23:1207–1212.26. Heald RJ, Moran BJ, Ryall RD, Sexton R, MacFarlane JK. Rectal cancer: the Basingstoke experience of total mesorectal excision, 1978-1997. Arch Surg. 1998; 133:894–899.27. Wibe A, Rendedal PR, Svensson E, Norstein J, Eide TJ, Myrvold HE, et al. Prognostic significance of the circumferential resection margin following total mesorectal excision for rectal cancer. Br J Surg. 2002; 89:327–334.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Surgery for Rectal Cancer
- Oncologic Results according to Operative Method after a Curative Resection for Low Rectal Cancers
- Multivisceral resection for locally advanced rectal cancer: adequate length of distal resection margin
- Omission of neoadjuvant radiotherapy for clinical T2/N1 and T3N0/1 middle and low rectal cancers with safe circumferential resection margins
- Association Between a Close Distal Resection Margin and Recurrence After a Sphincter-Saving Resection for T3 Mid- or Low-Rectal Cancer Without Radiotherapy