Ann Surg Treat Res.
2022 May;102(5):281-288. 10.4174/astr.2022.102.5.281.
Omission of neoadjuvant radiotherapy for clinical T2/N1 and T3N0/1 middle and low rectal cancers with safe circumferential resection margins
- Affiliations
-
- 1Department of Surgery, Chungnam National University Hospital, Daejeon, Korea
- KMID: 2529682
- DOI: http://doi.org/10.4174/astr.2022.102.5.281
Abstract
- Purpose
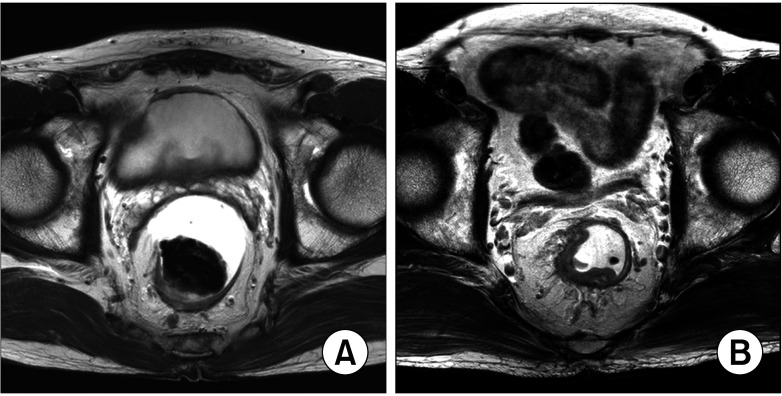
For moderately advanced rectal cancers with safe circumferential margins, the oncologic benefit of neoadjuvant radiotherapy must be reconsidered because of the possibility of overtreatment, resulting in complications from radiotoxicity. To evaluate the oncologic safety of the omission of neoadjuvant radiotherapy for moderately advanced rectal cancers, we evaluated and compared the prognoses of patients who underwent radical resection with and without neoadjuvant radiotherapy for T2/N1 and T3N0/1 middle and low rectal cancers with safe circumferential resection margins.
Methods
We retrospectively enrolled 66 patients who underwent radical resection for clinical (c) T2N1 and T3N0/1 middle and low rectal cancers between 2008 and 2014. Patients with distant metastasis; cT4, cN2, or positive lateral pelvic lymph nodes; positive circumferential resection margin; signet-ring cell carcinoma; cT1/2N0; or those who had received adjuvant radiotherapy were excluded. The clinical and pathological characteristics and 5-year oncologic outcomes of the noradiotherapy (n = 34) and radiotherapy (n = 32) groups were compared.
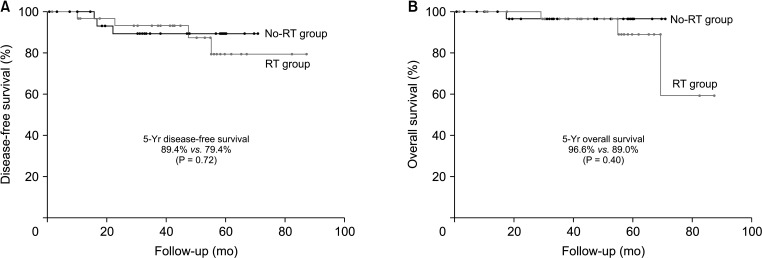
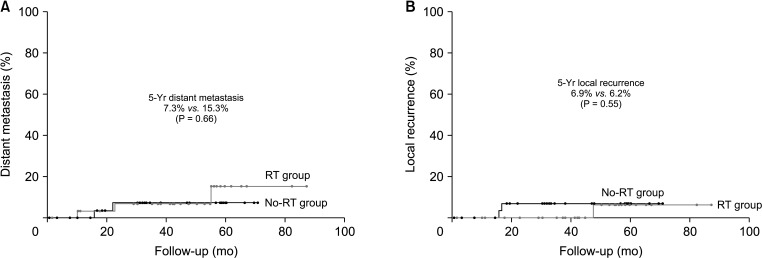
Results
The rates of abdominoperineal resection and ileostomies and the proportion of patients who received adjuvant chemotherapy were significantly higher in the radiotherapy group. There were no significant differences in tumor location, clinical stage, surgery type, pathologic N stage, anastomotic leakage, or long-term oncologic outcomes including 5-year disease-free survival, overall survival, and local recurrence and distant metastasis rates between both groups.
Conclusion
The oncologic benefit of neoadjuvant radiotherapy for cT2/N1 and T3N0/1 middle and low rectal cancers with safe circumferential resection margins is considered unclear, and it can be omitted to prevent radiotoxicity and facilitate prompt essential treatment.
Keyword
Figure
Reference
-
1. Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004; 351:1731–1740. PMID: 15496622.2. Bosset JF, Collette L, Calais G, Mineur L, Maingon P, Radosevic-Jelic L, et al. Chemotherapy with preoperative radiotherapy in rectal cancer. N Engl J Med. 2006; 355:1114–1123. PMID: 16971718.3. National Comprehensive Cancer Network (NCCN). NCCN Guidelines: rectal cancer, 2022 [Internet]. Plymouth Meeting, PA: NCCN;2022. cited 2022 Feb 17. Available from: https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1461 .4. Emmertsen KJ, Laurberg S. Low anterior resection syndrome score: development and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Ann Surg. 2012; 255:922–928. PMID: 22504191.5. Bregendahl S, Emmertsen KJ, Lindegaard JC, Laurberg S. Urinary and sexual dysfunction in women after resection with and without preoperative radiotherapy for rectal cancer: a population-based cross-sectional study. Colorectal Dis. 2015; 17:26–37. PMID: 25156386.6. Petrelli F, Trevisan F, Cabiddu M, Sgroi G, Bruschieri L, Rausa E, et al. Total neoadjuvant therapy in rectal cancer: a systematic review and meta-analysis of treatment outcomes. Ann Surg. 2020; 271:440–448. PMID: 31318794.7. Horvat N, Carlos Tavares Rocha C, Clemente Oliveira B, Petkovska I, Gollub MJ. MRI of rectal cancer: tumor staging, imaging techniques, and management. Radiographics. 2019; 39:367–387. PMID: 30768361.8. KSAR Study Group for Rectal Cancer. Essential items for structured reporting of rectal cancer MRI: 2016 consensus recommendation from the Korean Society of Abdominal Radiology. Korean J Radiol. 2017; 18:132–151. PMID: 28096724.9. Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med. 2001; 345:638–646. PMID: 11547717.10. Pommergaard HC, Gessler B, Burcharth J, Angenete E, Haglind E, Rosenberg J. Preoperative risk factors for anastomotic leakage after resection for colorectal cancer: a systematic review and meta-analysis. Colorectal Dis. 2014; 16:662–671. PMID: 24655784.11. Qin Q, Ma T, Deng Y, Zheng J, Zhou Z, Wang H, et al. Impact of preoperative radiotherapy on anastomotic leakage and stenosis after rectal cancer resection: post hoc analysis of a randomized controlled trial. Dis Colon Rectum. 2016; 59:934–942. PMID: 27602924.12. Mannaerts GH, Schijven MP, Hendrikx A, Martijn H, Rutten HJ, Wiggers T. Urologic and sexual morbidity following multimodality treatment for locally advanced primary and locally recurrent rectal cancer. Eur J Surg Oncol. 2001; 27:265–272. PMID: 11373103.13. Jimenez-Gomez LM, Espin-Basany E, Trenti L, Martí-Gallostra M, Sánchez-García JL, Vallribera-Valls F, et al. Factors associated with low anterior resection syndrome after surgical treatment of rectal cancer. Colorectal Dis. 2018; 20:195–200.14. Shin US, Kim CW, Yu CS, Kim JC. Delayed anastomotic leakage following sphincter-preserving surgery for rectal cancer. Int J Colorectal Dis. 2010; 25:843–849. PMID: 20387070.15. Bruheim K, Guren MG, Skovlund E, Hjermstad MJ, Dahl O, Frykholm G, et al. Late side effects and quality of life after radiotherapy for rectal cancer. Int J Radiat Oncol Biol Phys. 2010; 76:1005–1011. PMID: 19540058.16. Cercek A, Roxburgh CS, Strombom P, Smith JJ, Temple LK, Nash GM, et al. Adoption of total neoadjuvant therapy for locally advanced rectal cancer. JAMA Oncol. 2018; 4:e180071. PMID: 29566109.17. Folkesson J, Birgisson H, Pahlman L, Cedermark B, Glimelius B, Gunnarsson U. Swedish Rectal Cancer Trial: long lasting benefits from radiotherapy on survival and local recurrence rate. J Clin Oncol. 2005; 23:5644–5650. PMID: 16110023.18. Kusters M, Marijnen CA, van de Velde CJ, Rutten HJ, Lahaye MJ, Kim JH, et al. Patterns of local recurrence in rectal cancer; a study of the Dutch TME trial. Eur J Surg Oncol. 2010; 36:470–476. PMID: 20096534.19. Sauer R, Liersch T, Merkel S, Fietkau R, Hohenberger W, Hess C, et al. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J Clin Oncol. 2012; 30:1926–1933. PMID: 22529255.20. West NP, Finan PJ, Anderin C, Lindholm J, Holm T, Quirke P. Evidence of the oncologic superiority of cylindrical abdominoperineal excision for low rectal cancer. J Clin Oncol. 2008; 26:3517–3522. PMID: 18541901.21. Martling AL, Holm T, Rutqvist LE, Moran BJ, Heald RJ, Cedemark B. Effect of a surgical training programme on outcome of rectal cancer in the County of Stockholm. Stockholm Colorectal Cancer Study Group, Basingstoke Bowel Cancer Research Project. Lancet. 2000; 356:93–96. PMID: 10963244.22. Huh JW, Lim SW, Kim HR, Kim YJ. Effects of postoperative adjuvant radiotherapy on recurrence and survival in stage III rectal cancer. J Gastrointest Surg. 2011; 15:963–970. PMID: 21479672.23. Park IJ, Kim HC, Yu CS, Kim TW, Jang SJ, Kim JC. Effect of adjuvant radiotherapy on local recurrence in stage II rectal cancer. Ann Surg Oncol. 2008; 15:519–525. PMID: 17960464.24. Deng X, Liu P, Jiang D, Wei M, Wang X, Yang X, et al. Neoadjuvant radiotherapy versus surgery alone for stage II/III mid-low rectal cancer with or without high-risk factors: a prospective multicenter stratified randomized trial. Ann Surg. 2020; 272:1060–1069. PMID: 31599809.25. Jootun N, Sengupta S, Cunningham C, Charlton P, Betts M, Weaver A, et al. Neoadjuvant radiotherapy in rectal cancer: less is more? Colorectal Dis. 2020; 22:261–268. PMID: 31556218.26. Agger EA, Jörgren FH, Lydrup MA, Buchwald PL. Risk of local recurrence of rectal cancer and circumferential resection margin: population-based cohort study. Br J Surg. 2020; 107:580–585. PMID: 32133651.27. Detering R, Rutgers MLW, Bemelman WA, Hompes R, Tanis PJ. Prognostic importance of circumferential resection margin in the era of evolving surgical and multidisciplinary treatment of rectal cancer: a systematic review and meta-analysis. Surgery. 2021; 170:412–431. PMID: 33838883.28. Brown G, Davies S, Williams GT, Bourne MW, Newcombe RG, Radcliffe AG, et al. Effectiveness of preoperative staging in rectal cancer: digital rectal examination, endoluminal ultrasound or magnetic resonance imaging? Br J Cancer. 2004; 91:23–29. PMID: 15188013.29. Glynne-Jones R, Wyrwicz L, Tiret E, Brown G, Rödel C, Cervantes A, et al. Rectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017; 28(Suppl 4):iv22–iv40. PMID: 28881920.30. Marchegiani F, Palatucci V, Capelli G, Guerrieri M, Belluco C, Rega D, et al. Rectal sparing approach after neoadjuvant therapy in patients with rectal cancer: the preliminary results of the ReSARCh trial. Ann Surg Oncol. 2022; 29:1880–1889. PMID: 34855063.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Update and Debate Issues in Surgical Treatment of Middle and Low Rectal Cancer
- Long-term bowel functional outcomes following anal sphincter-preserving surgery for upper and middle rectal cancer: a single-center longitudinal study
- Risk factors for locoregional recurrence in patients with pathologic T3N0 rectal cancer with negative resection margin treated by surgery alone
- Prognostic Analysis According to N Stage and Circumferential Resection Margin in Patients with Locally Advanced Rectal Cancer
- Controversial issues in radiotherapy for rectal cancer: a systematic review