J Clin Neurol.
2009 Sep;5(3):151-152. 10.3988/jcn.2009.5.3.151.
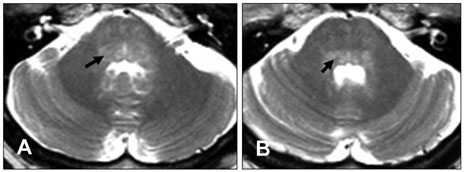
Anti-Ri-Antibody-Associated Paraneoplastic Syndrome in a Man with Breast Cancer Showing a Reversible Pontine Lesion on MRI
- Affiliations
-
- 1Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. kkkim@amc.seoul.kr
- KMID: 2045423
- DOI: http://doi.org/10.3988/jcn.2009.5.3.151
Abstract
- BACKGROUND
Paraneoplastic neurological disorders associated with anti-Ri-antibodies, which are typically present with opsoclonus-myoclonus-ataxia. Most cases with anti-Ri-antibodyassociated paraneoplastic syndrome due to breast cancer occur in women - its occurrence in men is extremely rare. CASE REPORT: We present herein the case of a male patient with breast cancer who had atypical anti-Ri-antibody-associated paraneoplastic syndrome presenting as complete horizontal ophthalmoplegia, left trigeminal sensory symptoms, and truncal ataxia. Following the diagnosis of paraneoplastic syndrome, chemotherapy and immunomodulating treatment including intravenous immunoglobulin and oral prednisolone were administered. Although the patient was negative for serum anti-Ri-antibodies 14 weeks later, his symptoms persisted. CONCLUSIONS: To our knowledge, this is the first case report of ophthalmoplegia without opsoclonus-myoclonus in a male anti-Ri-antibody-positive patient with breast cancer.
MeSH Terms
Figure
Cited by 1 articles
-
Two Cases of Seronegative Paraneoplastic Neurologic Syndrome with Opsoclonus Nystagmus
Seong Hoon Bae, Jeon Mi Lee, Sung Huhn Kim
Korean J Otorhinolaryngol-Head Neck Surg. 2019;62(6):355-360. doi: 10.3342/kjorl-hns.2018.00318.
Reference
-
1. Luque FA, Furneaux HM, Ferziger R, Rosenblum MK, Wray SH, Schold SC Jr, et al. Anti-Ri: an antibody associated with paraneoplastic opsoclonus and breast cancer. Ann Neurol. 1991. 29:241–251.
Article2. Escudero D, Barnadas A, Codina M, Fueyo J, Graus F. Anti-Ri-associated paraneoplastic neurologic disorder without opsoclonus in a patient with breast cancer. Neurology. 1993. 43:1605–1606.
Article3. Ohmer R, Golnik KC, Richards AI, Kosmorsky GS. Ophthalmoplegia associated with the anti-Ri antibody. J Neuroophthalmol. 1999. 19:246–248.
Article4. Voltz R. Paraneoplastic neurological syndromes: an update on diagnosis, pathogenesis, and therapy. Lancet Neurol. 2002. 1:294–305.
Article5. Wirtz PW, Sillevis Smitt PA, Hoff JI, de Leeuw B, Lammers GJ, van Duinen SG, et al. Anti-Ri antibody positive opsoclonus-myoclonus in a male patient with breast carcinoma. J Neurol. 2002. 249:1710–1712.
Article6. Pittock SJ, Lucchinetti CF, Lennon VA. Anti-neuronal nuclear autoantibody type 2: paraneoplastic accompaniments. Ann Neurol. 2003. 53:580–587.
Article7. Kastrup O, Meyring S, Diener HC. Atypical paraneoplastic brainstem encephalitis associated with anti-ri-antibodies due to thymic carcinoma with possible clinical response to immunoglobulins. Eur Neurol. 2001. 45:285–287.
Article8. Sutton IJ, Barnett MH, Watson JD, Ell JJ, Dalmau J. Paraneoplastic brainstem encephalitis and anti-Ri antibodies. J Neurol. 2002. 249:1597–1598.
Article9. Ko MW, Dalmau J, Galetta SL. Neuro-ophthalmologic manifestations of paraneoplastic syndromes. J Neuroophthalmol. 2008. 28:58–68.
Article10. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 9-1988. A 57-year-old woman with worsening opsoclonus. N Engl J Med. 1988. 318:563–570.11. Giordano SH, Cohen DS, Buzdar AU, Perkins G, Hortobagyi GN. Breast carcinoma in men: a population-based study. Cancer. 2004. 101:51–57.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anti-Yo-associated paraneoplastic cerebellar degeneration in a patient with chemotherapy-responsive ovarian cancer: A case report with a review of literatures
- Anti-Hu Antibody-Mediated Myelopathy Associated with Gastric Adenocarcinoma
- Myelitis Presenting Anti-Yo Antibody in a Patient with Prostatic Adenocarcinoma
- Two Cases of Seronegative Paraneoplastic Neurologic Syndrome with Opsoclonus Nystagmus
- Paraneoplastic Encephalitis Associated with Locally Advanced Human Epidermal Growth Factor Receptor 2-Positive Breast Cancer