Korean Circ J.
2009 Oct;39(10):434-438. 10.4070/kcj.2009.39.10.434.
Acute and Subacute Stent Thrombosis in a Patient With Clopidogrel Resistance: A Case Report
- Affiliations
-
- 1The Heart Research Center of Chonnam National University Hospital, Gwangju, Korea.
- 2Cardiovascular Research Institute of Chonnam National University, Gwangju, Korea.
- KMID: 2028925
- DOI: http://doi.org/10.4070/kcj.2009.39.10.434
Abstract
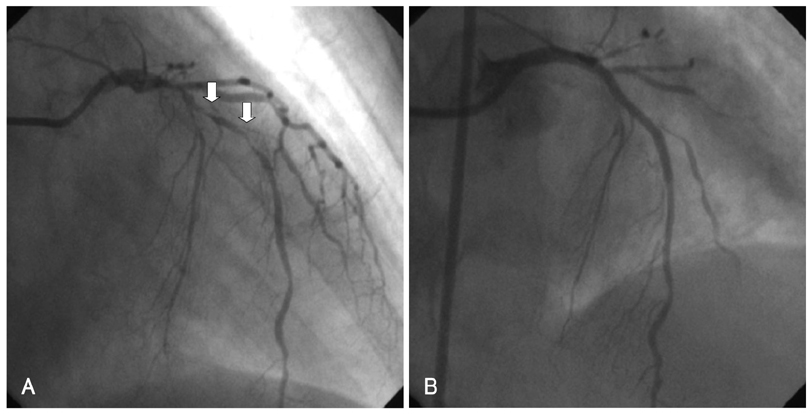
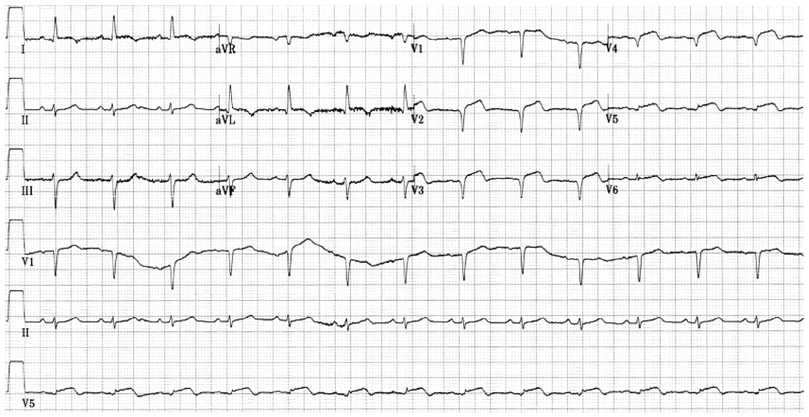
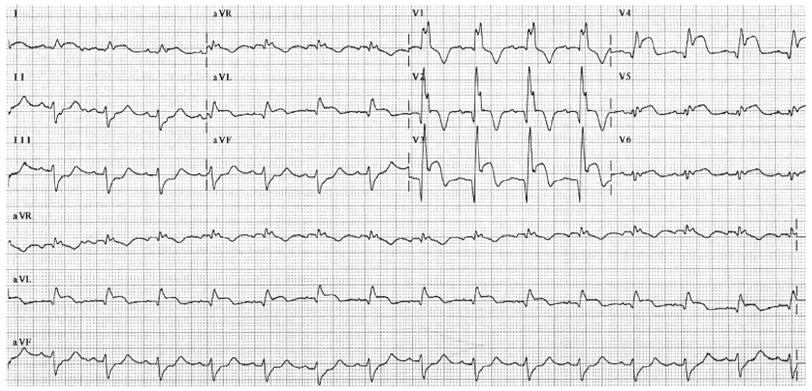
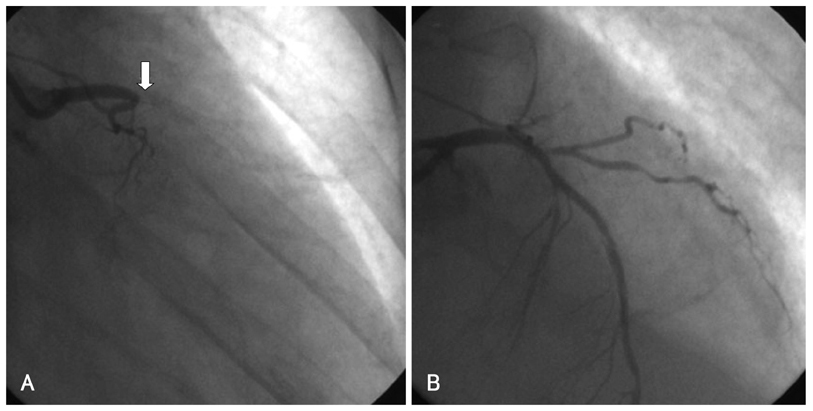
- Drug-eluting stents (DES) are considered the treatment of choice for most patients with obstructive coronary artery disease when percutaneous intervention (PCI) is feasible. However, stent thrombosis seems to occur more frequently with DES and occasionally is associated with resistance to anti-platelet drugs. We have experienced a case of recurrent stent thrombosis in a patient with clopidogrel resistance. A 63-year-old female patient suffered from acute myocardial infarction and underwent successful PCI of the left anterior descending coronary artery (LAD) with two DESs. She was found to be hyporesponsive to clopidogrel and was treated with triple anti-platelet therapy (aspirin 100 mg, clopidogrel 75 mg, and cilostazol 200 mg daily). Three days after discharge, she developed chest pain and was again taken to the cardiac catheterization laboratory, where coronary angiography (CAG) showed total occlusion of the mid-LAD where the stent had been placed. After intravenous administration of a glycoprotein IIb/IIIa inhibitor, balloon angioplasty was performed, resulting in Thrombolysis In Myocardial Infarction (TIMI) III antegrade flow. The next day, however, she complained of severe chest pain, and the electrocardiogram showed marked ST-segment elevation in V1-V6, I, and aVL with complete right bundle branch block. Emergent CAG revealed total occlusion of the proximal LAD due to stent thrombosis. She was successfully treated with balloon angioplasty and was discharged with triple anti-platelet therapy.
Keyword
MeSH Terms
-
Administration, Intravenous
Angioplasty, Balloon
Bundle-Branch Block
Cardiac Catheterization
Cardiac Catheters
Chest Pain
Coronary Angiography
Coronary Artery Disease
Coronary Vessels
Drug-Eluting Stents
Electrocardiography
Female
Glycoproteins
Humans
Middle Aged
Myocardial Infarction
Stents
Tetrazoles
Thrombosis
Ticlopidine
Glycoproteins
Tetrazoles
Ticlopidine
Figure
Reference
-
1. Serruys PW, Degertekin M, Tanabe K, et al. Intravascular ultrasound findings in the multicenter, randomized, double-blind RAVEL (Randomized study with the sirolimus-eluting Velocity balloon-expandable stent in the treatment of patients with de novo native coronary artery Lesions) trial. Circulation. 2002. 106:798–803.2. Colombo A, Drzewiecki J, Banning A, et al. Randomized study to assess the effectiveness of slow- and moderate-release polymer-based paclitaxel-eluting stents for coronary artery lesions. Circulation. 2003. 108:788–794.3. Zhang F, Ge J, Qian J, et al. Sirolimus-eluting stents in real-world patients with ST-segment elevation acute myocardial infarction. Int Heart J. 2007. 48:303–311.4. Kim JY, Yoon JH. Aspirin and clopidogrel resistance in drug eluting stent era. Korean Circ J. 2007. 37:135–147.5. Schuhlen H, Kastrati A, Pache J, Dirschinger J, Schomig A. Incidence of thrombotic occlusion and major adverse cardiac events between two and four weeks after coronary stent placement: analysis of 5,678 patients with a four-week ticlopidine regimen. J Am Coll Cardiol. 2001. 37:2066–2073.6. De la Torre-Hernandez JM, Alfonso F, Hernandez F, et al. Drug-eluting stent thrombosis: results from the multicenter Spanish registry ESTROFA (Estudio ESpanol sobre TROmbosis de stents FArmacoactivos). J Am Coll Cardiol. 2008. 51:986–990.7. Kuchulakanti , Chu WW, Torguson R, et al. Correlates and long-term outcomes of angiographically proven stent thrombosis with sirolimus-and paclitaxel-eluting stents. Circulation. 2006. 113:1108–1113.8. Park SH, Hong GR, Seo HS, Tahk SJ. Stent thrombosis after successful drug-eluting stent implantation. Korean Circ J. 2005. 35:163–171.9. Kim SS, Jeong MH, Sim DS, et al. Very late stent thrombosis of drug eluting stent after discontinuation of dual anti-platelet therapy in a patient treated with both drug eluting and bare metal stents. Korean Cir J. 2009. 39:205–208.10. Gum PA, Kottke-Marchant K, Poggio ED, et al. Profile and prevalence of aspirin resistance in patients with cardiovascular disease. Am J Cardiol. 2001. 88:230–235.11. Gurbel PA, Blinden KP, Hiatt BL, O'Connor CM. Clopidogrel for coronary stenting: response variability, drug resistance, and the effect of pretreatment platelet reactivity. Circulation. 2003. 107:2908–2913.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Ticagrelor Rescue Therapy in a Patient with Subacute Stent Thrombosis
- Significance of Clopidogrel Resistance Related to the Stent-Assisted Angioplasty in Patients with Atherosclerotic Cerebrovascular Disease
- Successful Prasugrel Rescue Therapy in Clopidogrel Resistant Patients Who Had Recurrent Stent Thrombosis of Drug-Eluting-Stent: The Role of Prasugrel in Clopidogrel Nonresponders
- Subacute In-stent Thrombosis after Carotid Artery Stenting: A Case Report
- Very Late Stent Thrombosis after Drug-Eluting Stent Implantation in a Patient without Aspirin and Clopidogrel Resistance