Korean Circ J.
2012 May;42(5):311-318. 10.4070/kcj.2012.42.5.311.
Prediction of Left Atrial Fibrosis With Speckle Tracking Echocardiography in Mitral Valve Disease: A Comparative Study With Histopathology
- Affiliations
-
- 1Division of Cardiology, Kangwon National University Hospital, Chuncheon, Korea.
- 2Gangnam Severance Hospital, Heart Center, Yonsei University College of Medicine, Seoul, Korea. choi0928@yuhs.ac
- 3Division of Cardiology, Yonsei Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 4Yonsei Cardiovascular Research Institute, Yonsei University College of Medicine, Seoul, Korea.
- 5Department of Cardiothoracic Surgery, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2028759
- DOI: http://doi.org/10.4070/kcj.2012.42.5.311
Abstract
- BACKGROUND AND OBJECTIVES
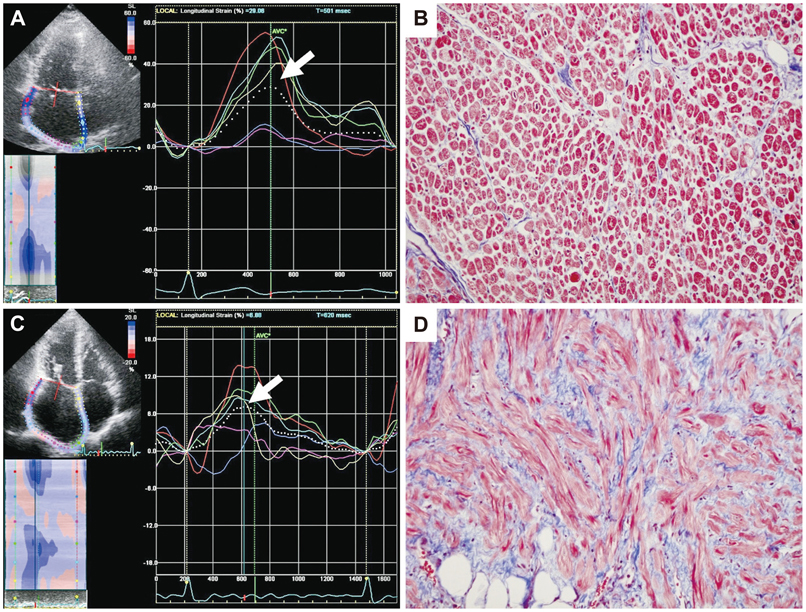
Left atrial (LA) fibrosis is a main determinant of LA remodeling and development of atrial fibrillation. However, non-invasive prediction of LA fibrosis is challenging. We investigated whether preoperative LA strain as measured by speckle tracking echocardiography could predict the degree of LA fibrosis and LA reverse remodeling after mitral valve (MV) surgery.
SUBJECTS AND METHODS
Speckle tracking echocardiography and LA volume measurements were performed in 50 patients one day before MV surgery. LA tissues were obtained during the surgery, and the degrees of their interstitial fibroses were measured. LA volume measurements were repeated within 30 days after surgery (n=50) and 1-year later (n=39).
RESULTS
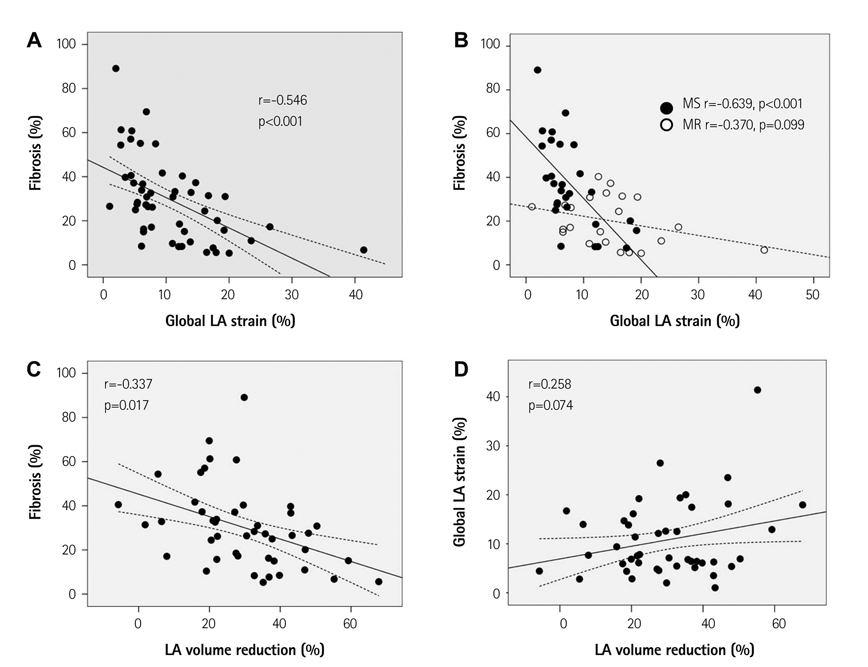
Left atrial global strain was significantly correlated with the degree of LA fibrosis (r=-0.55, p<0.001), and its correlation was independent of age, underlying rhythm, presence of rheumatic heart disease and type of predominant MV disease (B=-1.37, 95% confidence interval -2.32 - -0.41, p=0.006). The degree of LA fibrosis was significantly correlated with early (r=-0.337, p=0.017) and 1-year (r=-0.477, p=0.002) percent LA volume reduction after MV surgery, but LA global strain was not significant.
CONCLUSION
Left atrial strain as measured by speckle tracking echocardiography might be helpful for predicting the degree of LA fibrosis in patients with MV disease.
Keyword
MeSH Terms
Figure
Reference
-
1. Nattel S. Electrophysiologic remodeling: are ion channels static players or dynamic movers? J Cardiovasc Electrophysiol. 1999. 10:1553–1556.2. Abhayaratna WP, Seward JB, Appleton CP, et al. Left atrial size: physiologic determinants and clinical applications. J Am Coll Cardiol. 2006. 47:2357–2363.3. Cho DK, Ha JW, Chang BC, et al. Factors determining early left atrial reverse remodeling after mitral valve surgery. Am J Cardiol. 2008. 101:374–377.4. Casaclang-Verzosa G, Gersh BJ, Tsang TS. Structural and functional remodeling of the left atrium: clinical and therapeutic implications for atrial fibrillation. J Am Coll Cardiol. 2008. 51:1–11.5. Barnes ME, Miyasaka Y, Seward JB, et al. Left atrial volume in the prediction of first ischemic stroke in an elderly cohort without atrial fibrillation. Mayo Clin Proc. 2004. 79:1008–1014.6. Sanders P, Morton JB, Kistler PM, Vohra JK, Kalman JM, Sparks PB. Reversal of atrial mechanical dysfunction after cardioversion of atrial fibrillation: implications for the mechanisms of tachycardia-mediated atrial cardiomyopathy. Circulation. 2003. 108:1976–1984.7. Trikas A, Papathanasiou S, Tousoulis D, et al. Left atrial function, cytokines and soluble apoptotic markers in mitral stenosis: effects of valvular replacement. Int J Cardiol. 2005. 99:111–115.8. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005. 18:1440–1463.9. Sanfilippo AJ, Abascal VM, Sheehan M, et al. Atrial enlargement as a consequence of atrial fibrillation: a prospective echocardiographic study. Circulation. 1990. 82:792–797.10. Spencer KT, Mor-Avi V, Gorcsan J 3rd, et al. Effects of aging on left atrial reservoir, conduit, and booster pump function: a multi-institution acoustic quantification study. Heart. 2001. 85:272–277.11. Langeland S, D'hooge J, Wouters PF, et al. Experimental validation of a new ultrasound method for the simultaneous assessment of radial and longitudinal myocardial deformation independent of insonation angle. Circulation. 2005. 112:2157–2162.12. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986. 1:307–310.13. Cameli M, Caputo M, Mondillo S, et al. Feasibility and reference values of left atrial longitudinal strain imaging by two-dimensional speckle tracking. Cardiovasc Ultrasound. 2009. 7:6.14. Donal E, Ollivier R, Veillard D, et al. Left atrial function assessed by trans-thoracic echocardiography in patients treated by ablation for a lone paroxysmal atrial fibrillation. Eur J Echocardiogr. 2010. 11:845–852.15. Di Salvo G, Caso P, Lo Piccolo R, et al. Atrial myocardial deformation properties predict maintenance of sinus rhythm after external cardioversion of recent-onset lone atrial fibrillation: a color Doppler myocardial imaging and transthoracic and transesophageal echocardiographic study. Circulation. 2005. 112:387–395.16. Eshoo S, Boyd AC, Ross DL, Marwick TH, Thomas L. Strain rate evaluation of phasic atrial function in hypertension. Heart. 2009. 95:1184–1191.17. Shin MS, Kim BR, Oh KJ, et al. Echocardiographic assessments of left atrial strain and volume in healthy patients and patients with mitral valvular heart disease by tissue Doppler imaging and 3-dimensional echocardiography. Korean Circ J. 2009. 39:280–287.18. Donal E, Raud-Raynier P, De Place C, et al. Resting echocardiographic assessments of left atrial function and filling pressure interest in the understanding of exercise capacity in patients with chronic congestive heart failure. J Am Soc Echocardiogr. 2008. 21:703–710.19. Leung DY, Boyd A, Ng AA, Chi C, Thomas L. Echocardiographic evaluation of left atrial size and function: current understanding, pathophysiologic correlates, and prognostic implications. Am Heart J. 2008. 156:1056–1064.20. Vianna-Pinton R, Moreno CA, Baxter CM, Lee KS, Tsang TS, Appleton CP. Two-dimensional speckle-tracking echocardiography of the left atrium: feasibility and regional contraction and relaxation differences in normal subjects. J Am Soc Echocardiogr. 2009. 22:299–305.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Left Atrial Dissection after Mitral Valve Replacement Demonstrated by Transesophageal Echocardiography
- Relation between Atrial Fibrillation and Echocardiographic Size of Left Atrium
- Free-Floating Left Atrial Thrombus with Recurrent cerebral Embolic Event Associated Mitral Stenosis
- Left Atrial Mural Endocarditis Diagnosed by Transesophageal Echocardiography in a Patient with Mitral Valve Prolapse
- Left Atrial Dissection by Aorto-Left Atrial Fistula after Aortic Valve Replacement: A case report