J Korean Neurosurg Soc.
2012 Nov;52(5):484-487. 10.3340/jkns.2012.52.5.484.
Glioblastoma Multiforme with Subcutaneous Metastases, Case Report and Literature Review
- Affiliations
-
- 1Department of Neurosurgery, Renji Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China. qiuzhoub@hotmail.com
- 2Gamma-knife treatment Center, Renji Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China.
- KMID: 2018257
- DOI: http://doi.org/10.3340/jkns.2012.52.5.484
Abstract
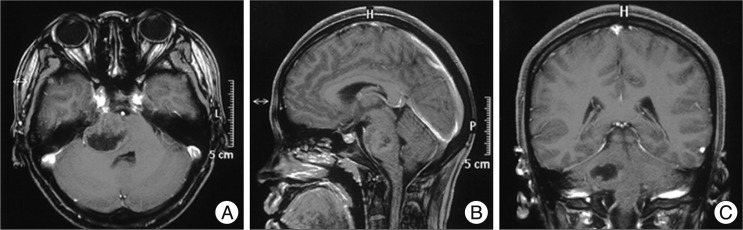
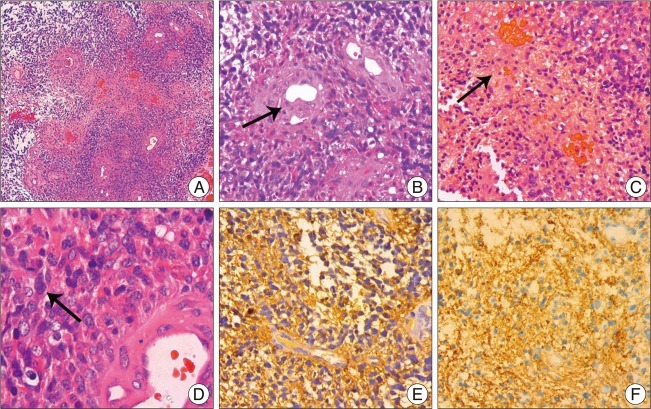
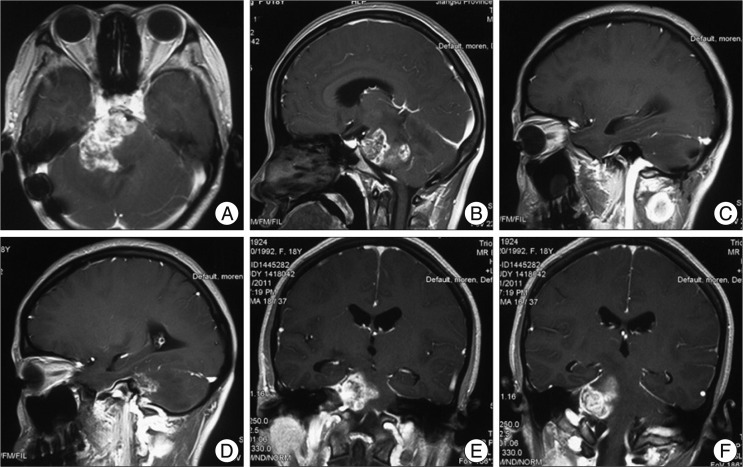
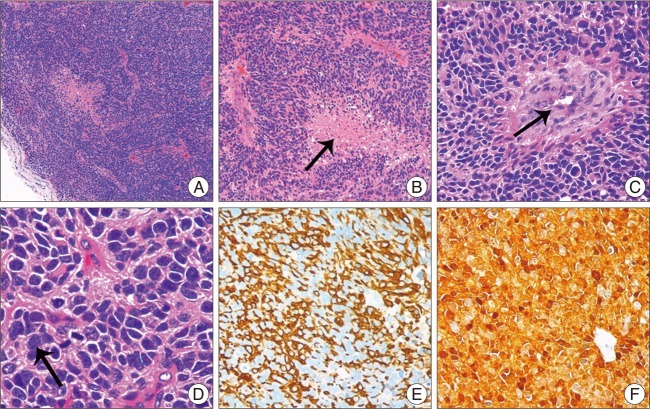
- Glioblastoma multiforme (GBM) is the most common primary brain tumor and the most malignant astrocytoma in adults, with rare extra-cranial metastases, especially for subcutaneous metastases. It could be easily misdiagnosed as primary subcutaneous tumor. In this report, we describe a patient with pontine GBM who developed a subcutaneous swelling at the ipsilateral posterior cervical region 8 months after operation, and the pathological and immunocytochemical examination carry the same characteristics as the primary intracranial GBM cells, which defined it as subcutaneous metastasis. GBM with subcutaneous metastasis is extremely rare, and knowledge of a prior intracranial GBM, pathological examinations and immunocytochemical tests with markers typically expressed by GBM are of vital importance for the diagnosis of GBM metastasis. Surgical resection of subcutaneous swelling, followed by chemotherapy and radiotherapy, could be the best strategy of treatment for the patients with GBM subcutaneous metastasis.
Keyword
Figure
Reference
-
1. Allan RS. Scalp metastasis from glioblastoma. J Neurol Neurosurg Psychiatry. 2004; 75:559. PMID: 15026496.2. Ates LE, Bayindir C, Bilgic B, Karasu A. Glioblastoma with lymph node metastases. Neuropathology. 2003; 23:146–149. PMID: 12777104.
Article3. Bouillot-Eimer S, Loiseau H, Vital A. Subcutaneous tumoral seeding from a glioblastoma following stereotactic biopsy : case report and review of the literature. Clin Neuropathol. 2005; 24:247–251. PMID: 16320817.4. Figueroa P, Lupton JR, Remington T, Olding M, Jones RV, Sekhar LN, et al. Cutaneous metastasis from an intracranial glioblastoma multiforme. J Am Acad Dermatol. 2002; 46:297–300. PMID: 11807444.
Article5. González Cámpora R, Otal Salaverri C, Vázquez Ramirez F, Salguero Villadiego M, Galera Davidson H. Metastatic glioblastoma multiforme in cervical lymph nodes. Report of a case with diagnosis by fine needle aspiration. Acta Cytol. 1993; 37:938–942. PMID: 8249517.6. Jain N, Mirakhur M, Flynn P, Choudhari KA. Cutaneous metastasis from glioblastoma. Br J Neurosurg. 2005; 19:65–68. PMID: 16147588.
Article7. Mentrikoski M, Johnson MD, Korones DN, Scott GA. Glioblastoma multiforme in skin : a report of 2 cases and review of the literature. Am J Dermatopathol. 2008; 30:381–384. PMID: 18645311.
Article8. Miliaras G, Tsitsopoulos PP, Markoula S, Kyritsis A, Polyzoidis KS, Malamou-Mitsi V. Multifocal glioblastoma with remote cutaneous metastasis : a case report and review of the literature. Cent Eur Neurosurg. 2009; 70:39–42. PMID: 19191206.
Article9. Moon KS, Jung S, Lee MC, Kim IY, Kim HW, Lee JK, et al. Metastatic glioblastoma in cervical lymph node after repeated craniotomies : report of a case with diagnosis by fine needle aspiration. J Korean Med Sci. 2004; 19:911–914. PMID: 15608410.
Article10. Saad AG, Sachs J, Turner CD, Proctor M, Marcus KJ, Wang L, et al. Extracranial metastases of glioblastoma in a child : case report and review of the literature. J Pediatr Hematol Oncol. 2007; 29:190–194. PMID: 17356401.11. Santos AV, Saraiva PF, Santiago B. [Extracranial metastasis of glioblastoma multiforme]. Acta Med Port. 2003; 16:209–211. PMID: 12868404.12. Steinbok P, Dolman CL, Goldie JH. Variation in response to CCNU of glioblastoma multiforme in brain and cervical lymph node. Case report. J Neurosurg. 1985; 62:918–921. PMID: 2987441.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Multicentric Glioblastoma Multiforme
- A Case of Meningioma Compatible with Metastatic Glioblastoma Multiforme
- A Case of Glioblastoma Multiforme of the Cerebellum
- Scalp Metastasis of Glioblastoma Multiforme after Craniotomy and stereotatic Interstitial Brachytherapy
- Intramedullary Glioblastoma Multiforme: Report of 3 Cases