J Periodontal Implant Sci.
2014 Jun;44(3):147-155. 10.5051/jpis.2014.44.3.147.
Anterior maxillary defect reconstruction with a staged bilateral rotated palatal graft
- Affiliations
-
- 1Department of Periodontology, Ewha Womans University Graduate School of Medicine, Seoul, Korea.
- 2Division of Oral and Maxillofacial Surgery, Department of Dentistry, Hanyang University College of Medicine, Seoul, Korea. fastchang@hanyang.ac.kr
- KMID: 2012990
- DOI: http://doi.org/10.5051/jpis.2014.44.3.147
Abstract
- PURPOSE
In the anterior maxilla, hard and soft tissue augmentations are sometimes required to meet esthetic and functional demands. In such cases, primary soft tissue closure after bone grafting procedures is indispensable for a successful outcome. This report describes a simple method for soft tissue coverage of a guided bone regeneration (GBR) site using the double-rotated palatal subepithelial connective tissue graft (RPSCTG) technique for a maxillary anterior defect.
METHODS
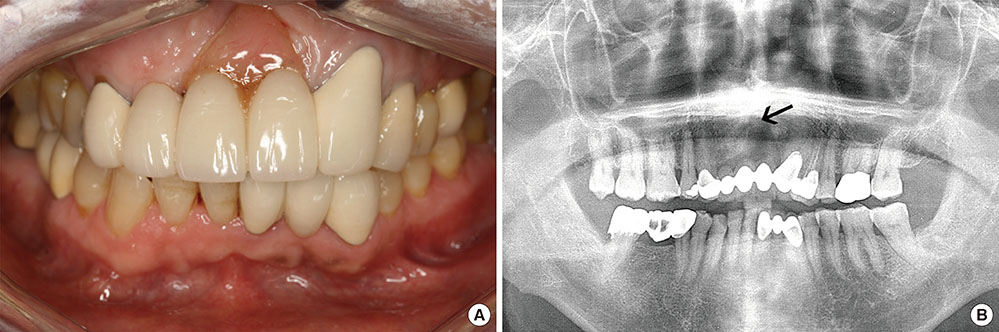
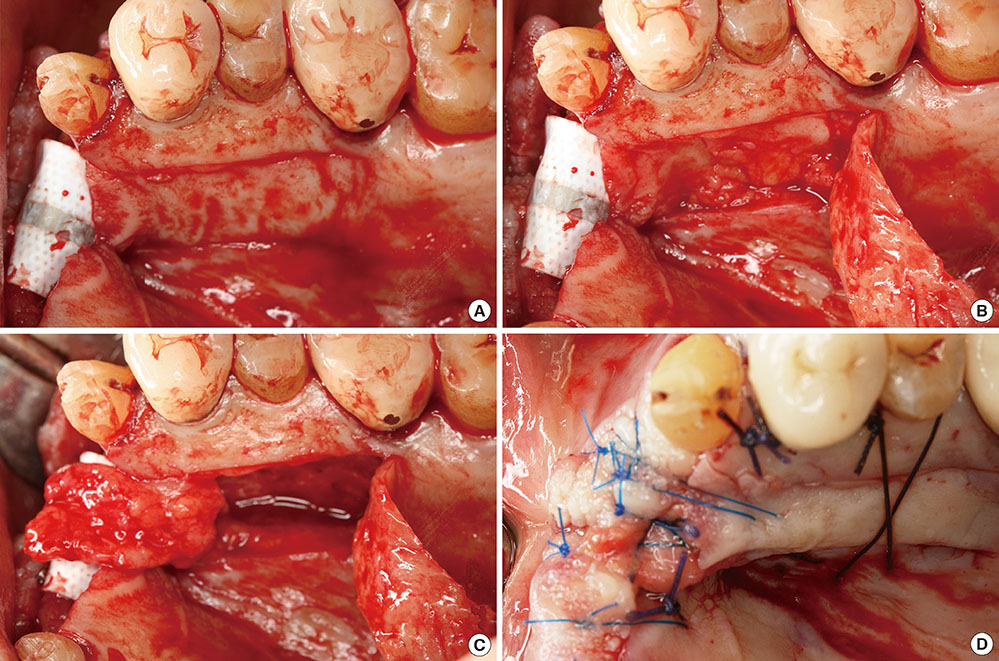
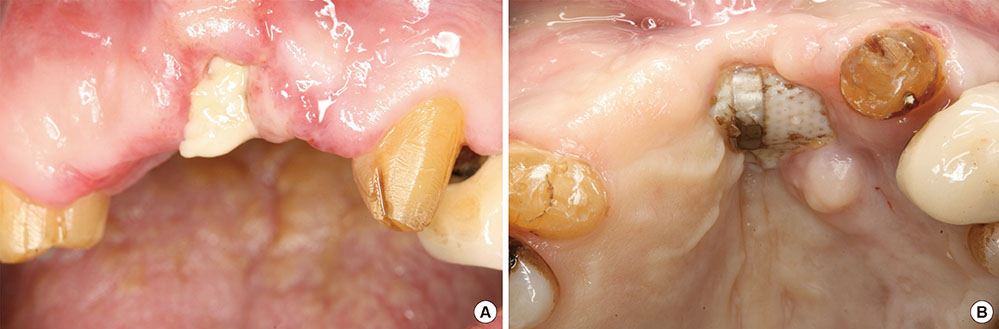
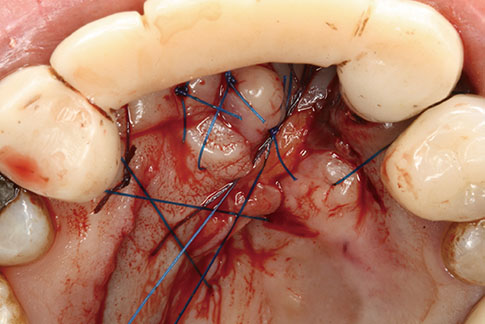
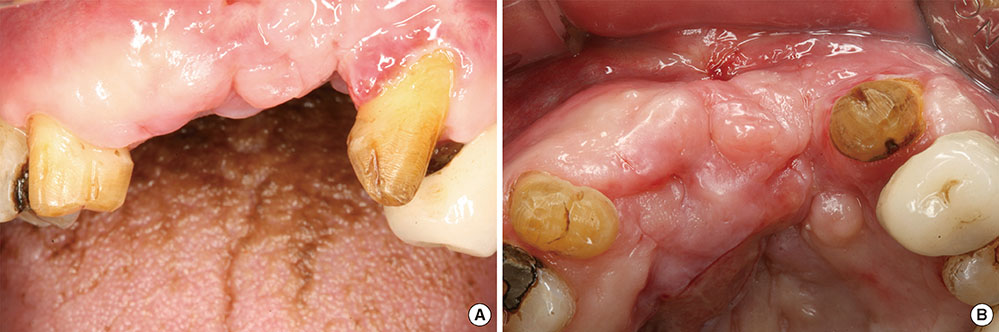
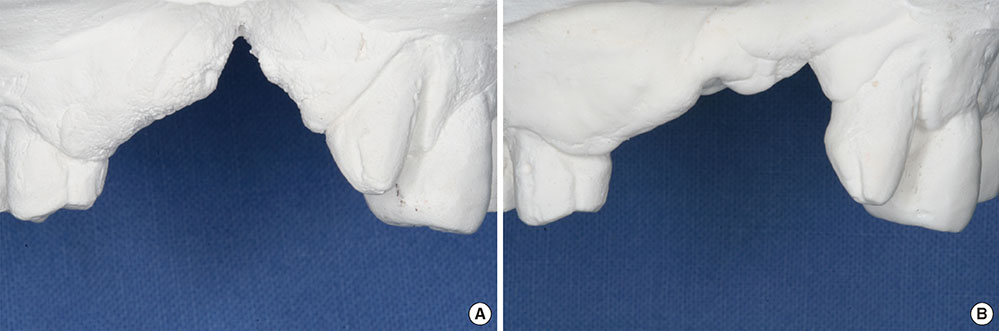
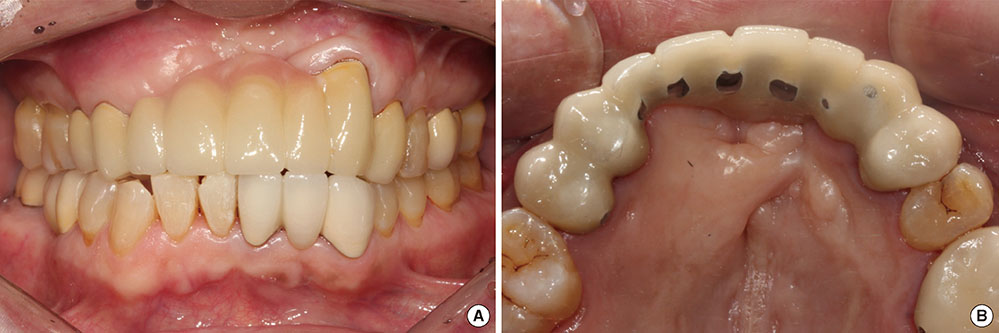
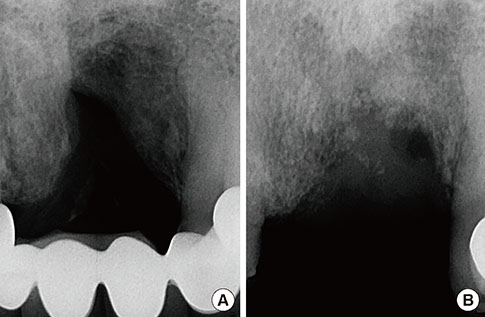
We present a 60-year-old man with a defect in the anterior maxilla requiring hard and soft tissue augmentations. The bone graft materials were filled above the alveolar defect and a titanium-reinforced nonresorbable membrane was placed to cover the graft materials. We used the RPSCTG technique to achieve primary soft tissue closure over the graft materials and the barrier membrane. Additional soft tissue augmentation using a contralateral RPSCTG and membrane removal were simultaneously performed 7 weeks after the stage 1 surgery to establish more abundant soft tissue architecture.
RESULTS
Flap necrosis occurred after the stage 1 surgery. Signs of infection or suppuration were not observed in the donor or recipient sites after the stage 2 surgery. These procedures enhanced the alveolar ridge volume, increased the amount of keratinized tissue, and improved the esthetic profile for restorative treatment.
CONCLUSIONS
The use of RPSCTG could assist the soft tissue closure of the GBR sites because it provides sufficient soft tissue thickness, an ample vascular supply, protection of anatomical structures, and patient comfort. The treatment outcome was acceptable, despite membrane exposure, and the RPSCTG allowed for vitalization and harmonization with the recipient tissue.
MeSH Terms
Figure
Reference
-
1. Carlsson GE, Bergman B, Hedegard B. Changes in contour of the maxillary alveolar process under immediate dentures: a longitudinal clinical and x-ray cephalometric study covering 5 years. Acta Odontol Scand. 1967; 25:45–75.
Article2. Pietrokovski J, Massler M. Alveolar ridge resorption following tooth extraction. J Prosthet Dent. 1967; 17:21–27.
Article3. Kois JC. Esthetic extraction site development: the biologic variables. Contemp Esthet Restor Pract. 1998; 2:10–18.4. Kois JC. Predictable single tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2001; 22:199–206.5. Bitter RN. A rotated palatal flap ridge preservation technique to enhance restorative and hard and soft tissue esthetics for tooth replacement in the anterior maxilla. Int J Periodontics Restorative Dent. 2010; 30:195–201.6. Buser D, Bragger U, Lang NP, Nyman S. Regeneration and enlargement of jaw bone using guided tissue regeneration. Clin Oral Implants Res. 1990; 1:22–32.
Article7. Buser D, Dula K, Belser UC, Hirt HP, Berthold H. Localized ridge augmentation using guided bone regeneration. II. Surgical procedure in the mandible. Int J Periodontics Restorative Dent. 1995; 15:10–29.8. Hermann JS, Buser D. Guided bone regeneration for dental implants. Curr Opin Periodontol. 1996; 3:168–177.9. Misch CM. Comparison of intraoral donor sites for onlay grafting prior to implant placement. Int J Oral Maxillofac Implants. 1997; 12:767–776.10. Chiapasco M, Abati S, Romeo E, Vogel G. Clinical outcome of autogenous bone blocks or guided bone regeneration with e-PTFE membranes for the reconstruction of narrow edentulous ridges. Clin Oral Implants Res. 1999; 10:278–288.
Article11. Oda T, Sawaki Y, Ueda M. Experimental alveolar ridge augmentation by distraction osteogenesis using a simple device that permits secondary implant placement. Int J Oral Maxillofac Implants. 2000; 15:95–102.12. Simion M, Baldoni M, Zaffe D. Jawbone enlargement using immediate implant placement associated with a split-crest technique and guided tissue regeneration. Int J Periodontics Restorative Dent. 1992; 12:462–473.13. Langer B, Calagna LJ. The subepithelial connective tissue graft: a new approach to the enhancement of anterior cosmetics. Int J Periodontics Restorative Dent. 1982; 2:22–33.14. Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985; 56:715–720.
Article15. Goldstein M, Boyan BD, Schwartz Z. The palatal advanced flap: a pedicle flap for primary coverage of immediately placed implants. Clin Oral Implants Res. 2002; 13:644–650.
Article16. Tinti C, Parma-Benfenati S. Coronally positioned palatal sliding flap. Int J Periodontics Restorative Dent. 1995; 15:298–310.17. Nemcovsky CE, Artzi Z, Moses O. Rotated split palatal flap for soft tissue primary coverage over extraction sites with immediate implant placement: description of the surgical procedure and clinical results. J Periodontol. 1999; 70:926–934.
Article18. Khoury F, Happe A. The palatal subepithelial connective tissue flap method for soft tissue management to cover maxillary defects: a clinical report. Int J Oral Maxillofac Implants. 2000; 15:415–418.19. Stajcic Z. The buccal fat pad in the closure of oro-antral communications: a study of 56 cases. J Craniomaxillofac Surg. 1992; 20:193–197.
Article20. Seibert JS. Reconstruction of deformed, partially edentulous ridges, using full thickness onlay grafts. Part II. Prosthetic/periodontal interrelationships. Compend Contin Educ Dent. 1983; 4:549–562.21. Herford AS, Cooper TC, Maiorana C, Cicciu M. Vascularized connective tissue flap for bone graft coverage. J Oral Implantol. 2011; 37:279–285.
Article22. Gelb DA. Immediate implant surgery: three-year retrospective evaluation of 50 consecutive cases. Int J Oral Maxillofac Implants. 1993; 8:388–399.23. Gher ME, Quintero G, Assad D, Monaco E, Richardson AC. Bone grafting and guided bone regeneration for immediate dental implants in humans. J Periodontol. 1994; 65:881–891.
Article24. Buser D, Dula K, Belser U, Hirt HP, Berthold H. Localized ridge augmentation using guided bone regeneration. 1. Surgical procedure in the maxilla. Int J Periodontics Restorative Dent. 1993; 13:29–45.25. Santana RB, de Mattos CM. Efficacy of vascularized periosteal membranes in providing soft tissue closure at grafted human maxillary extraction sites. Int J Oral Maxillofac Implants. 2009; 24:81–87.26. Rehrmann A. A method of closure of oroantral perforation. Dtsch Zahnarztl Z. 1936; 39:1136–1139.27. Rosenquist B. A comparison of various methods of soft tissue management following the immediate placement of implants into extraction sockets. Int J Oral Maxillofac Implants. 1997; 12:43–51.28. von Wowern N. Closure of oroantral fistula with buccal flap: Rehrmann versus Moczar. Int J Oral Surg. 1982; 11:156–165.29. Sclar AG. Soft tissue and esthetic considerations in implant therapy. Chicago: Quintessence Publishing Co.;2003.30. Fagan MC, Miller RE, Lynch SE, Kao RT. Simultaneous augmentation of hard and soft tissues for implant site preparation using recombinant human platelet-derived growth factor: a human case report. Int J Periodontics Restorative Dent. 2008; 28:37–43.31. Martinez-Garcia A, Bueno JM. Incisive vessel-based palatal flap for the reconstruction of anterior maxillary soft tissues. Int J Periodontics Restorative Dent. 2011; 31:83–89.32. Simion M, Baldoni M, Rossi P, Zaffe D. A comparative study of the effectiveness of e-PTFE membranes with and without early exposure during the healing period. Int J Periodontics Restorative Dent. 1994; 14:166–180.33. Lekholm U, Becker W, Dahlin C, Becker B, Donath K, Morrison E. The role of early versus late removal of GTAM membranes on bone formation at oral implants placed into immediate extraction sockets. An experimental study in dogs. Clin Oral Implants Res. 1993; 4:121–129.
Article34. Machtei EE, Cho MI, Dunford R, Norderyd J, Zambon JJ, Genco RJ. Clinical, microbiological, and histological factors which influence the success of regenerative periodontal therapy. J Periodontol. 1994; 65:154–161.
Article35. Lekovic V, Kenney EB, Kovacevic K, Carranza FA Jr. Evaluation of guided tissue regeneration in Class II furcation defects: a clinical re-entry study. J Periodontol. 1989; 60:694–698.36. Wennstrom JL. Mucogingival therapy. Ann Periodontol. 1996; 1:671–701.
Article37. Carnio J. Surgical reconstruction of interdental papilla using an interposed subepithelial connective tissue graft: a case report. Int J Periodontics Restorative Dent. 2004; 24:31–37.
Article38. Carnio J, Hallmon WW. A technique for augmenting the palatal connective tissue donor site: clinical case report and histologic evaluation. Int J Periodontics Restorative Dent. 2005; 25:257–263.39. Liu CL, Weisgold AS. Connective tissue graft: a classification for incision design from the palatal site and clinical case reports. Int J Periodontics Restorative Dent. 2002; 22:373–379.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reconstruction of palatal defect using palatal flap
- Intraoral Reconstruction using Palatal Island Flap
- Titanium mesh and pedicled buccal fat pad for the reconstruction of maxillary defect: case report
- Functional reconstruction of dento-palatal and maxillary defect using staged operation of prefabricated scapular free flap and dental implants
- Combined application of roll flap and combination onlay-interpositional graft to enhance esthetics of maxillary anterior fixed partial denture: A case report