J Korean Assoc Oral Maxillofac Surg.
2014 Aug;40(4):169-172. 10.5125/jkaoms.2014.40.4.169.
Comparative analysis of the amount of postoperative drainage after intraoral vertical ramus osteotomy and sagittal split ramus osteotomy
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Oral Science Research Institute, College of Dentistry, Yonsei University, Seoul, Korea. ysjoms@yuhs.ac
- KMID: 2005441
- DOI: http://doi.org/10.5125/jkaoms.2014.40.4.169
Abstract
OBJECTIVES
The purpose of this retrospective study was to compare the amount of postoperative drainage via closed suction drainage system after intraoral vertical ramus osteotomy (IVRO) and sagittal split ramus osteotomy (SSRO).
MATERIALS AND METHODS
We planned a retrospective cohort study of 40 patients selected from a larger group who underwent orthognathic surgery from 2007 to 2013. Mean age (range) was 23.95 (16 to 35) years. Patients who underwent bilateral IVRO or SSRO were categorized into group I or group II, respectively, and each group consisted of 20 patients. Closed suction drainage system was inserted in mandibular osteotomy sites to decrease swelling and dead space, and records of drainage amount were collected. The data were compared and analyzed with independent t-test.
RESULTS
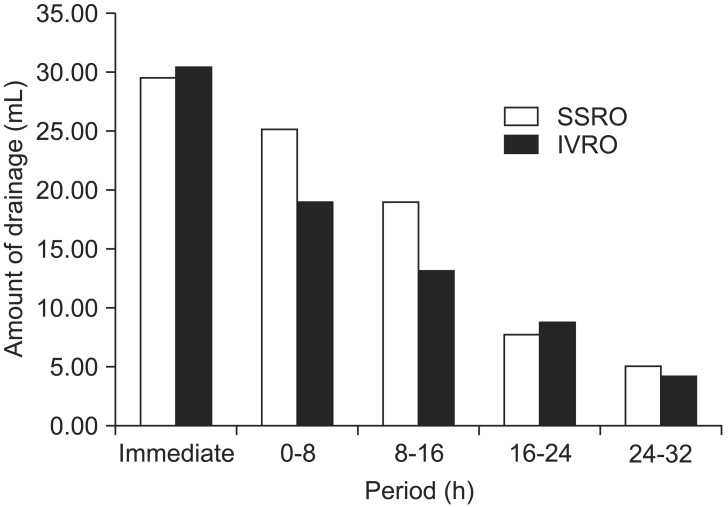
The closed suction drainage system was removed at 32 hours postoperatively, and the amount of drainage was recorded every 8 hours. In group I, the mean amount of drainage was 79.42 mL in total, with 31.20 mL, 19.90 mL, 13.90 mL, 9.47 mL, and 4.95 mL measured at 0, 8, 16, 24, and 32 hours postoperatively, respectively. In group II, the mean total amount of drainage was 90.11 mL, with 30.25 mL, 25.75 mL, 19.70 mL, 8.50 mL, and 5.91 mL measured at 0, 8, 16, 24, and 32 hours postoperatively, respectively. Total amount of drainage from group I was less than group II, but there was no statistically significant difference between the two groups (P=0.338). There was a significant difference in drainage between group I and group II only at 16 hours postoperatively (P=0.029).
CONCLUSION
IVRO and SSRO have different osteotomy design and different extent of medullary exposure; however, our results reveal that there is no remarkable difference in postoperative drainage of blood and exudate.
Keyword
MeSH Terms
Figure
Reference
-
1. Ovington LG. Dealing with drainage: the what, why, and how of wound exudate. Home Healthc Nurse. 2002; 20:368–374. PMID: 12055524.2. Jones J, Barraud J. An evaluation of KerraMax Care in the management of moderate to heavily exuding wounds. Br J Community Nurs. 2014; (Suppl):S48S50–S53. PMID: 24642740.
Article3. Politis C, Kunz S, Schepers S, Vrielinck L, Lambrichts I. Obstructive airway compromise in the early postoperative period after orthognathic surgery. J Craniofac Surg. 2012; 23:1717–1722. PMID: 23147331.
Article4. Hwang K, Kim HJ, Lee HS. Airway obstruction after orthognathic surgery. J Craniofac Surg. 2013; 24:1857–1858. PMID: 24036800.
Article5. Yoshioka I, Khanal A, Tominaga K, Horie A, Furuta N, Fukuda J. Vertical ramus versus sagittal split osteotomies: comparison of stability after mandibular setback. J Oral Maxillofac Surg. 2008; 66:1138–1144. PMID: 18486778.
Article6. Abou-Khalil R, Colnot C. Cellular and molecular bases of skeletal regeneration: what can we learn from genetic mouse models? Bone. 2014; 64:211–221. PMID: 24709685.
Article7. Clifton R, Haleem S, McKee A, Parker MJ. Closed suction surgical wound drainage after hip fracture surgery: a systematic review and meta-analysis of randomised controlled trials. Int Orthop. 2008; 32:723–727. PMID: 17687554.
Article8. He XD, Guo ZH, Tian JH, Yang KH, Xie XD. Whether drainage should be used after surgery for breast cancer? A systematic review of randomized controlled trials. Med Oncol. 2011; 28(Suppl 1):S22–S30. PMID: 20827578.
Article9. Ueki K, Marukawa K, Shimada M, Nakagawa K, Yamamoto E. The assessment of blood loss in orthognathic surgery for prognathia. J Oral Maxillofac Surg. 2005; 63:350–354. PMID: 15742286.
Article10. Morsi E. Continuous-flow cold therapy after total knee arthroplasty. J Arthroplasty. 2002; 17:718–722. PMID: 12216025.
Article11. Song G, Yang P, Hu J, Zhu S, Li Y, Wang Q. The effect of tranexamic acid on blood loss in orthognathic surgery: a meta-analysis of randomized controlled trials. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 115:595–600. PMID: 23260768.
Article12. Zellin G, Rasmusson L, Pålsson J, Kahnberg KE. Evaluation of hemorrhage depressors on blood loss during orthognathic surgery: a retrospective study. J Oral Maxillofac Surg. 2004; 62:662–666. PMID: 15170275.
Article13. Choi WS, Irwin MG, Samman N. The effect of tranexamic acid on blood loss during orthognathic surgery: a randomized controlled trial. J Oral Maxillofac Surg. 2009; 67:125–133. PMID: 19070758.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case report of hemifacial microsomia
- Surgical correction of maxillofacial deformity with fibrous-osseous lesion of mandible using the intraoral vertical ramus osteotomy
- Unilateral intraoral vertical ramus osteotomy and sagittal split ramus osteotomy for the treatment of asymmetric mandibles
- Stability after Surgical Correction of Mandibular Prognathism Using Bilateral Sagittal Split Ramus Osteotomy with Rigid Fixation
- Treatment of osteomyelitis in the rear area of the lingula of the mandible using sagittal split ramus osteotomy: a case report