Korean J Urol.
2014 Feb;55(2):91-96. 10.4111/kju.2014.55.2.91.
High-Intensity Focused Ultrasound as Salvage Therapy for Patients With Recurrent Prostate Cancer After Radiotherapy
- Affiliations
-
- 1Department of Urology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. besthml@medimail.co.kr
- KMID: 1988432
- DOI: http://doi.org/10.4111/kju.2014.55.2.91
Abstract
- PURPOSE
To evaluate the oncologic outcomes and postoperative complications of high-intensity focused ultrasound (HIFU) as a salvage therapy after external-beam radiotherapy (EBRT) failure in patients with prostate cancer.
MATERIALS AND METHODS
Between February 2002 and August 2010, we retrospectively reviewed the medical records of all patients who underwent salvage HIFU for transrectal ultrasound-guided, biopsy-proven locally recurred prostate cancer after EBRT failure (by ASTRO definition: prostate-specific antigen [PSA] failure after three consecutive PSA increases after a nadir, with the date of failure as the point halfway between the nadir date and the first increase or any increase great enough to provoke initiation of therapy). All patients underwent prostate magnetic resonance imaging and bone scintigraphy and had no evidence of distant metastasis. Biochemical recurrence (BCR) was defined according to the Stuttgart definition (PSA nadir plus 1.2 ng/mL).
RESULTS
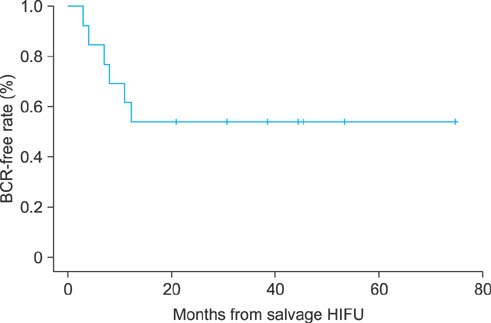
A total of 13 patients with a median age of 68 years (range, 60-76 years) were included. The median pre-EBRT PSA was 21.12 ng/mL, the pre-HIFU PSA was 4.63 ng/mL, and the period of salvage HIFU after EBRT was 32.7 months. The median follow-up after salvage HIFU was 44.5 months. The overall BCR-free rate was 53.8%. In the univariate analysis, predictive factors for BCR after salvage HIFU were higher pre-EBRT PSA (p=0.037), pre-HIFU PSA (p=0.015), and short time to nadir (p=0.036). In the multivariate analysis, there were no significant predictive factors for BCR. The complication rate requiring intervention was 38.5%.
CONCLUSIONS
Salvage HIFU for prostate cancer provides effective oncologic outcomes for local recurrence after EBRT failure. However, salvage HIFU had a relatively high rate of complications.
MeSH Terms
-
Follow-Up Studies
High-Intensity Focused Ultrasound Ablation
Humans
Magnetic Resonance Imaging
Medical Records
Multivariate Analysis
Neoplasm Metastasis
Postoperative Complications
Prostate*
Prostate-Specific Antigen
Prostatic Neoplasms*
Radionuclide Imaging
Radiotherapy*
Recurrence
Retrospective Studies
Salvage Therapy*
Ultrasonography*
Prostate-Specific Antigen
Figure
Reference
-
1. American Society for Therapeutic Radiology and Oncology Consensus Panel. Consensus statement: guidelines for PSA following radiation therapy. Int J Radiat Oncol Biol Phys. 1997; 37:1035–1041.2. Crouzet S, Murat FJ, Pasticier G, Cassier P, Chapelon JY, Gelet A. High intensity focused ultrasound (HIFU) for prostate cancer: current clinical status, outcomes and future perspectives. Int J Hyperthermia. 2010; 26:796–803.3. Ferlay J, Parkin DM, Steliarova-Foucher E. Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer. 2010; 46:765–781.4. Uchida T, Nakano M, Hongo S, Shoji S, Nagata Y, Satoh T, et al. High-intensity focused ultrasound therapy for prostate cancer. Int J Urol. 2012; 19:187–201.5. Acher PL, Thwaini A, Shergill IS, Barua JM. High-intensity focused ultrasound: a potential salvage treatment for recurrent prostate cancer following radiotherapy. Expert Rev Anticancer Ther. 2006; 6:969–970.6. Agarwal PK, Sadetsky N, Konety BR, Resnick MI, Carroll PR. Cancer of the Prostate Strategic Urological Research Endeavor (CaPSURE). Treatment failure after primary and salvage therapy for prostate cancer: likelihood, patterns of care, and outcomes. Cancer. 2008; 112:307–314.7. Uddin Ahmed H, Cathcart P, Chalasani V, Williams A, McCartan N, Freeman A, et al. Whole-gland salvage high-intensity focused ultrasound therapy for localized prostate cancer recurrence after external beam radiation therapy. Cancer. 2012; 118:3071–3078.8. Uchida T, Shoji S, Nakano M, Hongo S, Nitta M, Usui Y, et al. High-intensity focused ultrasound as salvage therapy for patients with recurrent prostate cancer after external beam radiation, brachytherapy or proton therapy. BJU Int. 2011; 107:378–382.9. Sanderson KM, Penson DF, Cai J, Groshen S, Stein JP, Lieskovsky G, et al. Salvage radical prostatectomy: quality of life outcomes and long-term oncological control of radiorecurrent prostate cancer. J Urol. 2006; 176:2025–2031.10. Rukstalis DB. Treatment options after failure of radiation therapy: a review. Rev Urol. 2002; 4:Suppl 2. S12–S17.11. Vallancien G, Prapotnich D, Cathelineau X, Baumert H, Rozet F. Transrectal focused ultrasound combined with transurethral resection of the prostate for the treatment of localized prostate cancer: feasibility study. J Urol. 2004; 171(6 Pt 1):2265–2267.12. Berge V, Baco E, Karlsen SJ. A prospective study of salvage high-intensity focused ultrasound for locally radiorecurrent prostate cancer: early results. Scand J Urol Nephrol. 2010; 44:223–227.13. Crouzet S, Murat FJ, Pommier P, Poissonnier L, Pasticier G, Rouviere O, et al. Locally recurrent prostate cancer after initial radiation therapy: early salvage high-intensity focused ultrasound improves oncologic outcomes. Radiother Oncol. 2012; 105:198–202.14. Zacharakis E, Ahmed HU, Ishaq A, Scott R, Illing R, Freeman A, et al. The feasibility and safety of high-intensity focused ultrasound as salvage therapy for recurrent prostate cancer following external beam radiotherapy. BJU Int. 2008; 102:786–792.15. D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998; 280:969–974.16. Trumbeckas D, Milonas D, Jievaltas M, Danilevicius M, Matjosaitis AJ. Influence of catheter on urinary flow during urodynamic pressure-flow study in men with symptomatic benign prostatic hyperplasia. Medicina (Kaunas). 2006; 42:15–21.17. Kelly CE. Evaluation of voiding dysfunction and measurement of bladder volume. Rev Urol. 2004; 6:Suppl 1. S32–S37.18. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.19. Agarwal PK, Sammon J, Bhandari A, Dabaja A, Diaz M, Dusik-Fenton S, et al. Safety profile of robot-assisted radical prostatectomy: a standardized report of complications in 3317 patients. Eur Urol. 2011; 59:684–698.20. Breeuwsma AJ, Pruim J, van den Bergh AC, Leliveld AM, Nijman RJ, Dierckx RA, et al. Detection of local, regional, and distant recurrence in patients with psa relapse after external-beam radiotherapy using (11)C-choline positron emission tomography. Int J Radiat Oncol Biol Phys. 2010; 77:160–164.21. Rosser CJ, Kuban DA, Levy LB, Chichakli R, Pollack A, Lee AK, et al. Prostate specific antigen bounce phenomenon after external beam radiation for clinically localized prostate cancer. J Urol. 2002; 168:2001–2005.22. Murat FJ, Poissonnier L, Rabilloud M, Belot A, Bouvier R, Rouviere O, et al. Mid-term results demonstrate salvage high-intensity focused ultrasound (HIFU) as an effective and acceptably morbid salvage treatment option for locally radiorecurrent prostate cancer. Eur Urol. 2009; 55:640–647.23. Nguyen PL, D'Amico AV, Lee AK, Suh WW. Patient selection, cancer control, and complications after salvage local therapy for postradiation prostate-specific antigen failure: a systematic review of the literature. Cancer. 2007; 110:1417–1428.24. Kimura M, Mouraviev V, Tsivian M, Mayes JM, Satoh T, Polascik TJ. Current salvage methods for recurrent prostate cancer after failure of primary radiotherapy. BJU Int. 2010; 105:191–201.25. Touma NJ, Izawa JI, Chin JL. Current status of local salvage therapies following radiation failure for prostate cancer. J Urol. 2005; 173:373–379.26. Gelet A, Chapelon JY, Poissonnier L, Bouvier R, Rouviere O, Curiel L, et al. Local recurrence of prostate cancer after external beam radiotherapy: early experience of salvage therapy using high-intensity focused ultrasonography. Urology. 2004; 63:625–629.27. Sung HH, Jeong BC, Seo SI, Jeon SS, Choi HY, Lee HM. Seven years of experience with high-intensity focused ultrasound for prostate cancer: advantages and limitations. Prostate. 2012; 72:1399–1406.28. Ganzer R, Robertson CN, Ward JF, Brown SC, Conti GN, Murat FJ, et al. Correlation of prostate-specific antigen nadir and biochemical failure after high-intensity focused ultrasound of localized prostate cancer based on the Stuttgart failure criteria-analysis from the @-Registry. BJU Int. 2011; 108(8 Pt 2):E196–E201.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Focused ultrasound and prostate cancer
- A structured framework for optimizing high-intensity focused ultrasound ablative treatment in localized prostate cancer
- Radiotherapy for prostate cancer
- Salvage Radiotherapy for Patients with PSA Relapse Following Radical Prostatectomy: Issues and Challenges
- Pain during Transrectal Ultrasound-Guided Prostate Biopsy and the Role of Periprostatic Nerve Block: What Radiologists Should Know