J Cardiovasc Ultrasound.
2011 Dec;19(4):224-227. 10.4250/jcu.2011.19.4.224.
Importance of Clinical and Echocardiographic Hemodynamic Assessment in Chronic Pulmonary Embolism
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Seoul National University College of Medicine, Seoul National University Hospital, Seoul, Korea. hkkim73@snu.ac.kr
- KMID: 1980389
- DOI: http://doi.org/10.4250/jcu.2011.19.4.224
Abstract
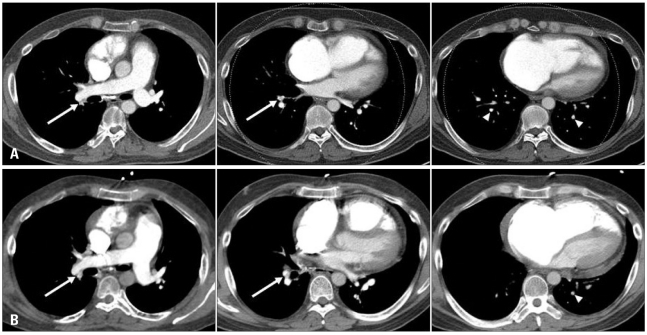
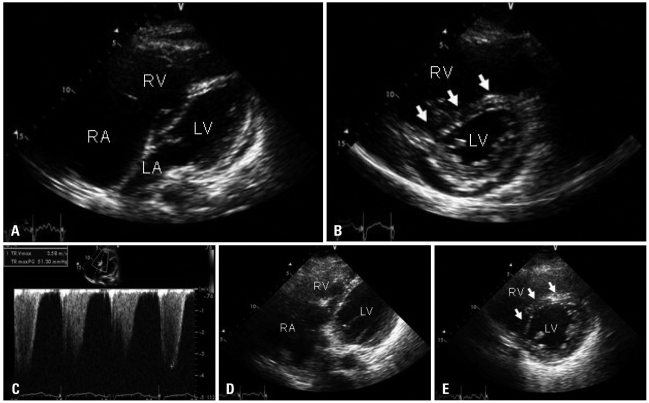
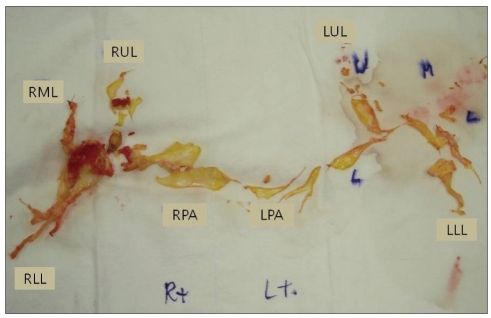
- We describe a 42-year-old man presenting to the emergency department with cardiogenic shock. He had a prior history of acute pulmonary embolism (PE), and had been on anticoagulation for 2 years. Although computed tomographic pulmonary angiography performed at the emergency department showed no change in the extent of PE and did not support a role of surgical treatment, pulmonary embolectomy was recommended by attending physician based on clinical and echocardiographic hemodynamic findings like unstable vital sign and markedly enlarged right ventricle with severely depressed systolic function. Surgery confirmed the presence of fresh thrombi. After surgery, hemodynamic status was progressively improved, but the patient died due to pneumonia and pulmonary hemorrhage.
MeSH Terms
Figure
Reference
-
1. Kucher N, Rossi E, De Rosa M, Goldhaber SZ. Massive pulmonary embolism. Circulation. 2006; 113:577–582. PMID: 16432055.2. Schoepf UJ, Goldhaber SZ, Costello P. Spiral computed tomography for acute pulmonary embolism. Circulation. 2004; 109:2160–2167. PMID: 15136509.3. Stein PD, Fowler SE, Goodman LR, Gottschalk A, Hales CA, Hull RD, Leeper KV Jr, Popovich J Jr, Quinn DA, Sos TA, Sostman HD, Tapson VF, Wakefield TW, Weg JG, Woodard PK. PIOPED II Investigators. Multidetector computed tomography for acute pulmonary embolism. N Engl J Med. 2006; 354:2317–2327. PMID: 16738268.4. Wells PS, Anderson DR, Rodger M, Ginsberg JS, Kearon C, Gent M, Turpie AG, Bormanis J, Weitz J, Chamberlain M, Bowie D, Barnes D, Hirsh J. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost. 2000; 83:416–420. PMID: 10744147.5. Henzler T, Barraza JM Jr, Nance JW Jr, Costello P, Krissak R, Fink C, Schoepf UJ. CT imaging of acute pulmonary embolism. J Cardiovasc Comput Tomogr. 2011; 5:3–11. PMID: 21051309.6. Come PC. Echocardiographic evaluation of pulmonary embolism and its response to therapeutic interventions. Chest. 1992; 101:151S–162S. PMID: 1555480.7. Lee JH, Park JH. Role of Echocardiography in Patients with Acute Pulmonary Thromboembolism. J Cardiovasc Ultrasound. 2008; 16:9–16.8. Casazza F, Bongarzoni A, Capozi A, Agostoni O. Regional right ventricular dysfunction in acute pulmonary embolism and right ventricular infarction. Eur J Echocardiogr. 2005; 6:11–14. PMID: 15664548.9. Kurzyna M, Torbicki A, Pruszczyk P, Burakowska B, Fijałkowska A, Kober J, Oniszh K, Kuca P, Tomkowski W, Burakowski J, Wawrzyńska L. Disturbed right ventricular ejection pattern as a new Doppler echocardiographic sign of acute pulmonary embolism. Am J Cardiol. 2002; 90:507–511. PMID: 12208411.10. Kucher N, Luder CM, Dörnhöfer T, Windecker S, Meier B, Hess OM. Novel management strategy for patients with suspected pulmonary embolism. Eur Heart J. 2003; 24:366–376. PMID: 12581684.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Acute Pulmonary Embolism After Cesarean Section Confirmed by Echocardiography
- Clinical Year in Review of Pulmonary Vascular Disease
- Chronic Thromboembolic Pulmonary Hypertension: Endovascular Treatment
- Pulmonary Artery Angiosarcoma Confused with Acute Pulmonary Thromboembolism: Focusing on Clinical and Echocardiographic Features in the Differentiation of Two Categories
- The treatment of the pulmonary embolism with tissue plasminogen activator: A case report