Preliminary three-dimensional analysis of tooth movement and arch dimension change of the maxillary dentition in Class II division 1 malocclusion treated with first premolar extraction: conventional anchorage vs. mini-implant anchorage
- Affiliations
-
- 1Department of Orthodontics, School of Dentistry, Dental Research Institute, Seoul National University, Seoul, Korea. drwhite@unitel.co.kr
- 2Smile Future Dental Clinic, Seoul, Korea.
- KMID: 1976680
- DOI: http://doi.org/10.4041/kjod.2012.42.6.280
Abstract
OBJECTIVE
This study aimed to compare the effects of conventional and orthodontic mini-implant (OMI) anchorage on tooth movement and arch-dimension changes in the maxillary dentition in Class II division 1 (CII div.1) patients.
METHODS
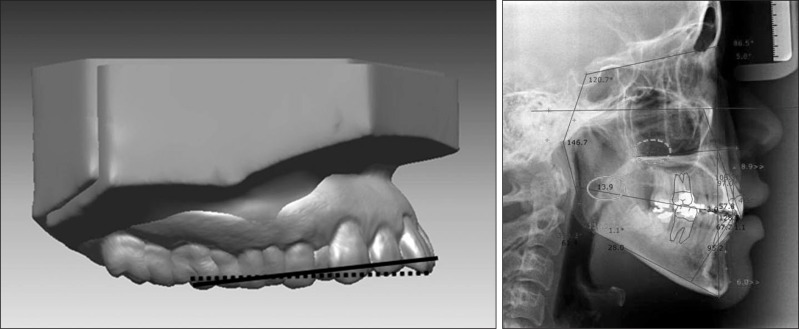
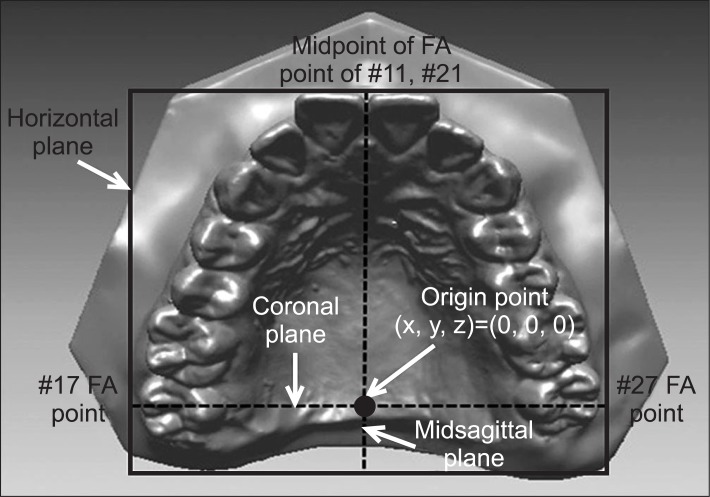
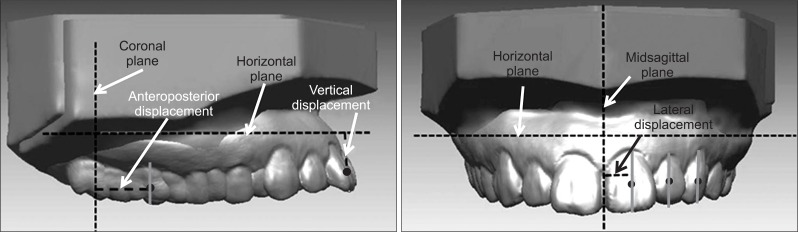
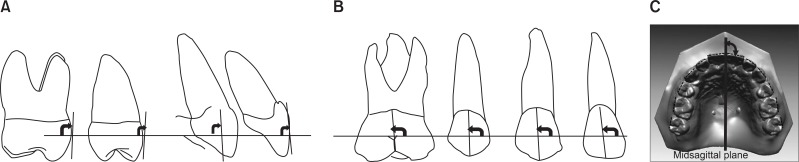
CII div.1 patients treated with extraction of the maxillary first and mandibular second premolars and sliding mechanics were allotted to conventional anchorage group (CA, n = 12) or OMI anchorage group (OA, n = 12). Pre- and post-treatment three-dimensional virtual maxillary models were superimposed using the best-fit method. Linear, angular, and arch-dimension variables were measured with software program. Mann-Whitney U-test and Wilcoxon signed-rank test were performed for statistical analysis.
RESULTS
Compared to the CA group, the OMI group showed more backward movement of the maxillary central and lateral incisors and canine (MXCI, MXLI, MXC, respectively; 1.6 mm, p < 0.001; 0.9 mm, p < 0.05; 1.2 mm, p < 0.001); more intrusion of the MXCI and MXC (1.3 mm, 0.5 mm, all p < 0.01); less forward movement of the maxillary second premolar, first, and second molars (MXP2, MXM1, MXM2, respectively; all 1.0 mm, all p < 0.05); less contraction of the MXP2 and MXM1 (0.7 mm, p < 0.05; 0.9 mm, p < 0.001); less mesial-in rotation of the MXM1 and MXM2 (2.6degrees, 2.5degrees, all p < 0.05); and less decrease of the inter-MXP2, MXM1, and MXM2 widths (1.8 mm, 1.5 mm, 2.0 mm, all p < 0.05).
CONCLUSIONS
In treatment of CII div.1 malocclusion, OA provided better anchorage and less arch-dimension change in the maxillary posterior teeth than CA during en-masse retraction of the maxillary anterior teeth.
Keyword
Figure
Cited by 4 articles
-
Finite element analysis of maxillary incisor displacement during en-masse retraction according to orthodontic mini-implant position
Jae-Won Song, Joong-Ki Lim, Kee-Joon Lee, Sang-Jin Sung, Youn-Sic Chun, Sung-Seo Mo
Korean J Orthod. 2016;46(4):242-252. doi: 10.4041/kjod.2016.46.4.242.Three-dimensional evaluation of tooth movement in Class II malocclusions treated without extraction by orthodontic mini-implant anchorage
Dler Ali, Hnd Mohammed, Seung-Hwan Koo, Kyung-Hwa Kang, Sang-Cheol Kim
Korean J Orthod. 2016;46(5):280-289. doi: 10.4041/kjod.2016.46.5.280.Three-dimensional analysis of tooth movement in Class II malocclusion treatment using arch wire with continuous tip-back bends and intermaxillary elastics
Ji-Yea Lee, Sung-Kwon Choi, Tae-Hoon Kwon, Kyung-Hwa Kang, Sang-Cheol Kim
Korean J Orthod. 2019;49(6):349-359. doi: 10.4041/kjod.2019.49.6.349.Quantitative evaluation of alveolar cortical bone density in adults with different vertical facial types using cone-beam computed tomography
Fulya Ozdemir, Murat Tozlu, Derya Germec Cakan
Korean J Orthod. 2014;44(1):36-43. doi: 10.4041/kjod.2014.44.1.36.
Reference
-
1. Redmond WR. Digital models: a new diagnostic tool. J Clin Orthod. 2001; 35:386–387. PMID: 11494942.2. Cha BK, Lee JY, Jost-Brinkmann PG, Yoshida N. Analysis of tooth movement in extraction cases using three-dimensional reverse engineering technology. Eur J Orthod. 2007; 29:325–331. PMID: 17513876.
Article3. Lai EH, Yao CC, Chang JZ, Chen I, Chen YJ. Three-dimensional dental model analysis of treatment outcomes for protrusive maxillary dentition: comparison of headgear, miniscrew, and miniplate skeletal anchorage. Am J Orthod Dentofacial Orthop. 2008; 134:636–645. PMID: 18984395.
Article4. Cho MY, Choi JH, Lee SP, Baek SH. Three-dimensional analysis of the tooth movement and arch dimension changes in Class I malocclusions treated with first premolar extractions: a guideline for virtual treatment planning. Am J Orthod Dentofacial Orthop. 2010; 138:747–757. PMID: 21130334.
Article5. Peavy DC Jr, Kendrick GS. The effects of tooth movement on the palatine rugae. J Prosthet Dent. 1967; 18:536–542. PMID: 5234941.
Article6. Hoggan BR, Sadowsky C. The use of palatal rugae for the assessment of anteroposterior tooth movements. Am J Orthod Dentofacial Orthop. 2001; 119:482–488. PMID: 11343019.
Article7. Christou P, Kiliaridis S. Vertical growth-related changes in the positions of palatal rugae and maxillary incisors. Am J Orthod Dentofacial Orthop. 2008; 133:81–86. PMID: 18174076.
Article8. Andrews LF. The six keys to normal occlusion. Am J Orthod. 1972; 62:296–309. PMID: 4505873.
Article9. Creekmore TD. Where teeth should be positioned in the face and jaws and how to get them there. J Clin Orthod. 1997; 31:586–608. PMID: 9511546.10. Ziegler P, Ingervall B. A clinical study of maxillary canine retraction with a retraction spring and with sliding mechanics. Am J Orthod Dentofacial Orthop. 1989; 95:99–106. PMID: 2916474.
Article11. Thiruvenkatachari B, Pavithranand A, Rajasigamani K, Kyung HM. Comparison and measurement of the amount of anchorage loss of the molars with and without the use of implant anchorage during canine retraction. Am J Orthod Dentofacial Orthop. 2006; 129:551–554. PMID: 16627183.
Article12. Upadhyay M, Yadav S, Nagaraj K, Nanda R. Dentoskeletal and soft tissue effects of mini-implants in Class II division 1 patients. Angle Orthod. 2009; 79:240–247. PMID: 19216590.
Article13. Upadhyay M, Yadav S, Patil S. Mini-implant anchorage for en-masse retraction of maxillary anterior teeth: a clinical cephalometric study. Am J Orthod Dentofacial Orthop. 2008; 134:803–810. PMID: 19061808.
Article14. Koh SA, Im WH, Park SH, Chun YS. Comparison of finite element analysis of the closing patterns between first and second premolar extraction spaces. Korean J Orthod. 2007; 37:407–420.15. Ong HB, Woods MG. An occlusal and cephalometric analysis of maxillary first and second premolar extraction effects. Angle Orthod. 2001; 71:90–102. PMID: 11302594.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Three-dimensional evaluation of tooth movement in Class II malocclusions treated without extraction by orthodontic mini-implant anchorage
- Correction of a maxillary canine-first premolar transposition using mini-implant anchorage
- Effect of maxillary premolar extraction on transverse arch dimension in Class III surgical-orthodontic treatment
- Directional forces using skeletal anchorage for treatment of skeletal Class II div.1 malocclusion
- Spatial changes of the upper dentition following en-masse space closure: A comparison between first and second premolar extraction