Biologic stability of plasma ion-implanted miniscrews
- Affiliations
-
- 1Private Practice, Seoul, Korea.
- 2Department of Orthodontics, School of Dentistry, Yonsei University, Seoul, Korea. yumichael@yuhs.ac
- 3Department of Oral Biology, School of Dentistry, Yonsei University, Seoul, Korea.
- KMID: 1975126
- DOI: http://doi.org/10.4041/kjod.2013.43.3.120
Abstract
OBJECTIVE
To gain basic information regarding the biologic stability of plasma ion-implanted miniscrews and their potential clinical applications.
METHODS
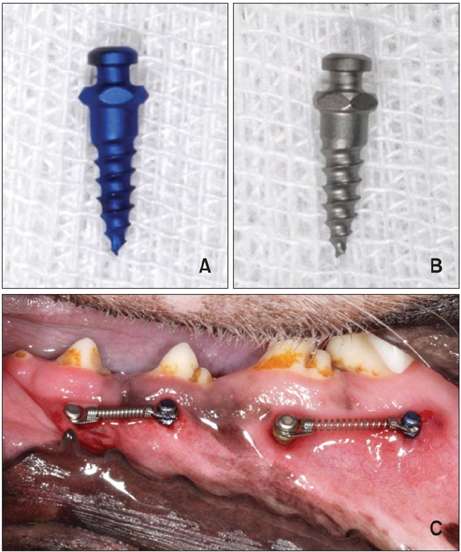
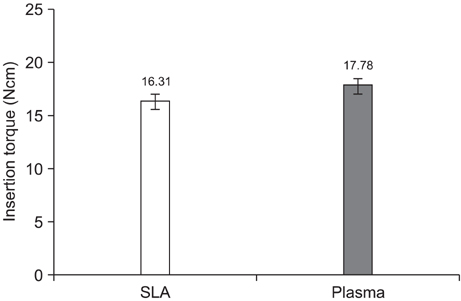
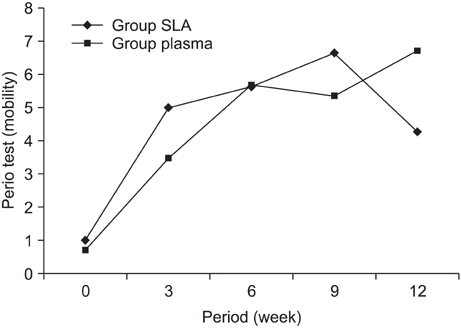
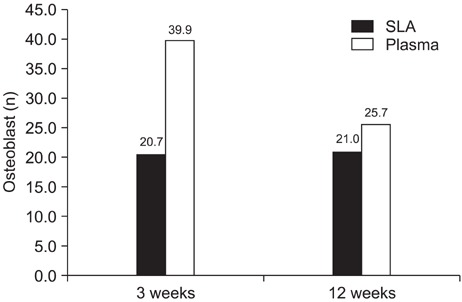
Sixteen plasma ion-implanted and 16 sandblasted and acid-etched (SLA) miniscrews were bilaterally inserted in the mandibles of 4 beagles (2 miniscrews of each type per quadrant). Then, 250 - 300 gm of force from Ni-Ti coil springs was applied for 2 different periods: 12 weeks on one side and 3 weeks contralaterally. Thereafter, the animals were sacrificed and mandibular specimens including the miniscrews were collected. The insertion torque and mobility were compared between the groups. The bone-implant contact and bone volume ratio were calculated within 800 microm of the miniscrews and compared between the loading periods. The number of osteoblasts was also quantified. The measurements were expressed as percentages and analyzed by independent t-tests (p < 0.05).
RESULTS
No significant differences in any of the analyzed parameters were noted between the groups.
CONCLUSIONS
The preliminary findings indicate that plasma ion-implanted miniscrews have similar biologic characteristics to SLA miniscrews in terms of insertion torque, mobility, bone-implant contact rate, and bone volume rate.
MeSH Terms
Figure
Cited by 3 articles
-
Stress distributions in peri-miniscrew areas from cylindrical and tapered miniscrews inserted at different angles
Sung-Hwan Choi, Seong-Jin Kim, Kee-Joon Lee, Sang-Jin Sung, Youn-Sic Chun, Chung-Ju Hwang
Korean J Orthod. 2016;46(4):189-198. doi: 10.4041/kjod.2016.46.4.189.Effects of recycling on the biomechanical characteristics of retrieved orthodontic miniscrews
Soon-Dong Yun, Sung-Hwan Choi, Jung-Yul Cha, Hyung-Seog Yu, Kwang-Mahn Kim, Jin Kim, Chung-Ju Hwang
Korean J Orthod. 2017;47(4):238-247. doi: 10.4041/kjod.2017.47.4.238.Incorporation of silver nanoparticles on the surface of orthodontic microimplants to achieve antimicrobial properties
Adith Venugopal, Nallal Muthuchamy, Harsh Tejani, Anantha-Iyengar Gopalan, Kwang-Pill Lee, Heon-Jin Lee, Hee Moon Kyung
Korean J Orthod. 2017;47(1):3-10. doi: 10.4041/kjod.2017.47.1.3.
Reference
-
1. Wehrbein H, Merz BR, Diedrich P, Glatzmaier J. The use of palatal implants for orthodontic anchorage. Design and clinical application of the orthosystem. Clin Oral Implants Res. 1996. 7:410–416.
Article2. Park YC, Lee SY, Kim DH, Jee SH. Intrusion of posterior teeth using mini-screw implants. Am J Orthod Dentofacial Orthop. 2003. 123:690–694.
Article3. Miyawaki S, Koyama I, Inoue M, Mishima K, Sugahara T, Takano-Yamamoto T. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2003. 124:373–378.
Article4. Chen CH, Chang CS, Hsieh CH, Tseng YC, Shen YS, Huang IY, et al. The use of microimplants in orthodontic anchorage. J Oral Maxillofac Surg. 2006. 64:1209–1213.
Article5. Cheng SJ, Tseng IY, Lee JJ, Kok SH. A prospective study of the risk factors associated with failure of mini-implants used for orthodontic anchorage. Int J Oral Maxillofac Implants. 2004. 19:100–106.6. Büchter A, Wiechmann D, Koerdt S, Wiesmann HP, Piffko J, Meyer U. Load-related implant reaction of mini-implants used for orthodontic anchorage. Clin Oral Implants Res. 2005. 16:473–479.
Article7. Joos U, Büchter A, Wiesmann HP, Meyer U. Strain driven fast osseointegration of implants. Head Face Med. 2005. 1:6.
Article8. Huja SS, Litsky AS, Beck FM, Johnson KA, Larsen PE. Pull-out strength of monocortical screws placed in the maxillae and mandibles of dogs. Am J Orthod Dentofacial Orthop. 2005. 127:307–313.
Article9. Habig KH. Friction and wear of sliding couples coated with TiC, TiN or TiB2. Surf Coat Technol. 1990. 42:133–147.
Article10. Kim SY, Moon YP, Park GH, Jo HH, Kim WG, Son MK, et al. Surface characteristics and electrochemical behaviors of TiN and ZrN coated orthodontic mini-screw. J Korean Ins Surf Eng. 2008. 41:232–239.
Article11. Albrektsson T, BråNemark PI, Hansson HA, Lindström J. Osseointegrated titanium implant. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981. 52:155–170.
Article12. Han CH, Johansson CB, Wennerberg A, Albrektsson T. Quantitative and qualitative investigations of surface enlarged titanium and titanium alloy implants. Clin Oral Implants Res. 1998. 9:1–10.
Article13. Buser D, Schenk RK, Steinemann S, Fiorellini JP, Fox CH, Stich H. Influence of surface characteristics on bone integration of titanium implants. A histomorphometric study in miniature pigs. J Biomed Mater Res. 1991. 25:889–902.
Article14. Kim HM, Miyaji F, Kokubo T, Nakamura T. Preparation of bioactive Ti and its alloys via simple chemical surface treatment. J Biomed Mater Res. 1996. 32:409–417.
Article15. Sul YT, Johansson CB, Jeong Y, Wennerberg A, Albrektsson T. Resonance frequency and removal torque analysis of implants with turned and anodized surface oxides. Clin Oral Implants Res. 2002. 13:252–259.
Article16. Byon E, Moon S, Cho SB, Jeong CY, Jeong Y, Sul YT. Electrochemical property and apatite formation of metal ion implanted titanium for medical implants. Surf Coat Technol. 2005. 200:1018–1021.
Article17. Wilson AD, Leyland A, Matthews A. A comparative study of the influence of plasma treatments, PVD coatings and ion implantation on the tribological performance of Ti-6Al-4V. Surf Coat Technol. 1999. 114:70–80.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A study on titanium miniscrew as orthodontic anchorage: An experimental investigation in dogs
- Influence of immediate loading on the removal torque value of mini-screws
- Histomorphometric evaluation of the bone surrounding orthodontic miniscrews according to their adjacent root proximity
- A study on the bone thickness of midpalatal suture area for miniscrew insertion
- Enhanced compatibility and initial stability of Ti6Al4V alloy orthodontic miniscrews subjected to anodization, cyclic precalcification, and heat treatment