J Adv Prosthodont.
2011 Mar;3(1):1-9. 10.4047/jap.2011.3.1.1.
Strain of implants depending on occlusion types in mandibular implant-supported fixed prostheses
- Affiliations
-
- 1Department of Prosthodontics and Dental Research Institute, Seoul National University Dental Hospital, School of Dentistry, Seoul National University, Seoul, Korea. lsuyoung@hanmail.net
- KMID: 1975107
- DOI: http://doi.org/10.4047/jap.2011.3.1.1
Abstract
- PURPOSE
This study investigated the strain of implants using a chewing simulator with strain gauges in mandibular implant-supported fixed prostheses under various dynamic loads.
MATERIALS AND METHODS
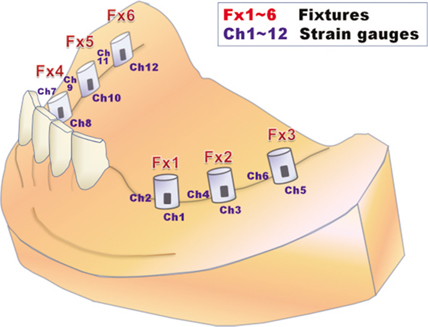
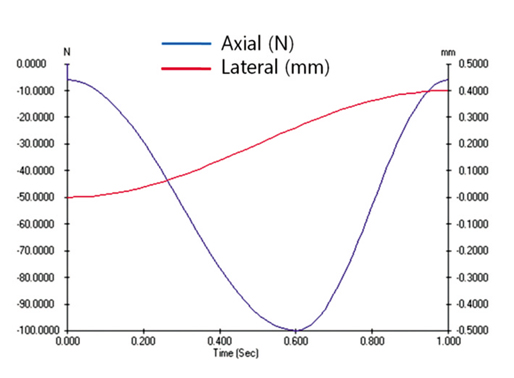
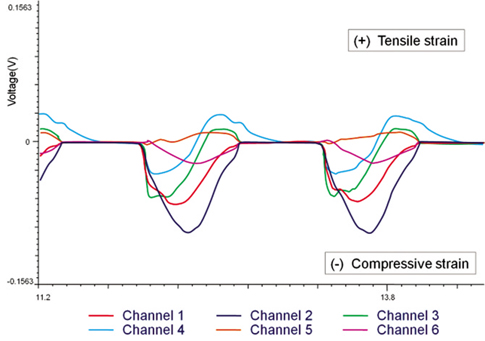
Three implant-supported 5-unit fixed prostheses were fabricated with three different occlusion types (Group I: Canine protected occlusion, Group II: Unilaterally balanced occlusion, Group III: Bilaterally balanced occlusion). Two strain gauges were attached to each implant abutment. The programmed dynamic loads (0 - 300 N) were applied using a chewing simulator (MTS 858 Mini Bionix II systems, MTS systems corp., Minn, USA) and the strains were monitored. The statistical analyses were performed using the paired t-test and the ANOVA.
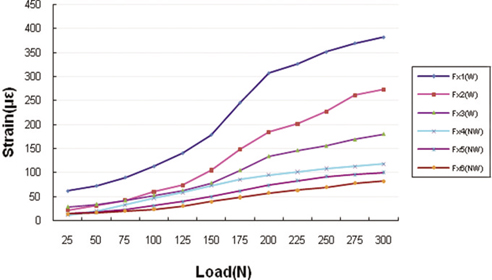
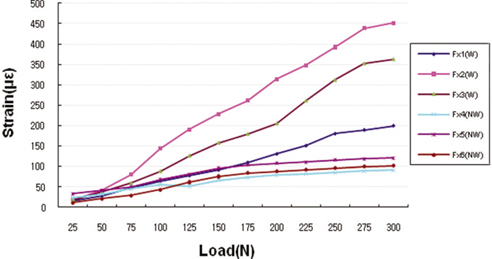
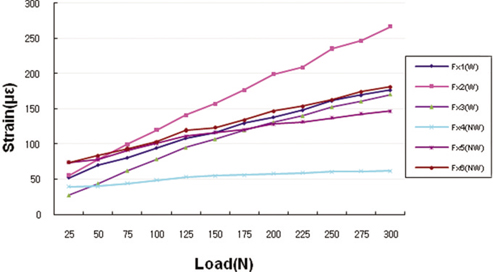
RESULTS
The mean strain values (MSV) for the working sides were 151.83 microepsilon, 176.23 microepsilon, and 131.07 microepsilon for Group I, Group II, and Group III, respectively. There was a significant difference between Group II and Group III (P < .05). Also, the MSV for non-working side were 58.29 microepsilon, 72.64 microepsilon, and 98.93 microepsilon for Group I, Group II, and Group III, respectively. One was significantly different from the others with a 95% confidence interval (P < .05).
CONCLUSION
The MSV for the working side of Groups I and II were significantly different from that for the non-working side (Group I: t = 7.58, Group II: t = 6.25). The MSV for the working side of Group II showed significantly larger than that of Group III (P < .01). Lastly, the MSV for the non-working side of Group III showed significantly larger than those of Group I or Group II (P < .01).
Figure
Reference
-
1. Adell R, Eriksson B, Lekholm U, Brånemark PI, Jemt T. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants. 1990. 5:347–359.2. Brånemark PI, Zarb GA, Albrektsson T, editors. Tissue Integrated Prostheses: osseointegration in clinical dentistry. 1985. Chicago: Quintessence;175–186.3. Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981. 10:387–416.4. Esposito M, Hirsch JM, Lekholm U, Thomsen P. Biological factors contributing to failures of osseointegrated oral implants. (II). Etiopathogenesis. Eur J Oral Sci. 1998. 106:721–764.5. Kohavi D. Complications in the tissue integrated prostheses components: clinical and mechanical evaluation. J Oral Rehabil. 1993. 20:413–422.6. Taylor TD, Agar JR, Vogiatzi T. Implant prosthodontics: current perspective and future directions. Int J Oral Maxillofac Implants. 2000. 15:66–75.7. Chapman RJ. Principles of occlusion for implant prostheses: guidelines for position, timing, and force of occlusal contacts. Quintessence Int. 1989. 20:473–480.8. Ashman RB, Van Buskirk WC. The elastic properties of a human mandible. Adv Dent Res. 1987. 1:64–67.9. Geng JP, Tan KB, Liu GR. Application of finite element analysis in implant dentistry: a review of the literature. J Prosthet Dent. 2001. 85:585–598.10. Gibbs CH, Mahan PE, Lundeen HC, Brehnan K, Walsh EK, Holbrook WB. Occlusal forces during chewing and swallowing as measured by sound transmission. J Prosthet Dent. 1981. 46:443–449.11. Bidez MW, Misch CE. Force transfer in implant dentistry: basic concepts and principles. J Oral Implantol. 1992. 18:264–274.12. Stanford CM, Brand RA. Toward an understanding of implant occlusion and strain adaptive bone modeling and remodeling. J Prosthet Dent. 1999. 81:553–561.13. Roberts WE. Naert I, van Steenberghe D, Worthington P, editors. Fundamental principles of bone physiology, metabolism and loading. Osseointegration in oral rehabilitation: an introductory textbook. 1993. London: Quintessence;163–164.14. Duyck J, Rønold HJ, Van Oosterwyck H, Naert I, Vander Sloten J, Ellingsen JE. The influence of static and dynamic loading on marginal bone reactions around osseointegrated implants: an animal experimental study. Clin Oral Implants Res. 2001. 12:207–218.15. Quirynen M, Naert I, van Steenberghe D. Fixture design and overload influence marginal bone loss and fixture success in the Brånemark system. Clin Oral Implants Res. 1992. 3:104–111.16. Horshaw SJ, Brunski JB, Cochran GV. Mechanical loading of Brånemark implants affects interfacial bone modelling and remodelling. Int J Oral Maxillofac Implants. 1994. 9:345–360.17. Frost HM. Wolff's Law and bone's structural adaptations to mechanical usage: an overview for clinicians. Angle Orthod. 1994. 64:175–188.18. Pilliar RM, Deporter DA, Watson PA, Valiquette N. Dental implant design-effect on bone remodeling. J Biomed Mater Res. 1991. 25:467–483.19. Buser D, Nydegger T, Hirt HP, Cochran DL, Nolte LP. Removal torque values of titanium implants in the maxilla of miniature pigs. Int J Oral Maxillofac Implants. 1998. 13:611–619.20. Hebel KS, Gajjar RC. Cement-retained versus screw-retained implant restorations: achieving optimal occlusion and esthetics in implant dentistry. J Prosthet Dent. 1997. 77:28–35.21. Mericske-Stern R, Venetz E, Fahrländer F, Bürgin W. In vivo force measurements on maxillary implants supporting a fixed prosthesis or an overdenture: a pilot study. J Prosthet Dent. 2000. 84:535–547.22. Bergendal T, Engquist B. Implant-supported overdentures: a longitudinal prospective study. Int J Oral Maxillofac Implants. 1998. 13:253–262.23. Lekholm U, Gunne J, Henry P, Higuchi K, Lindén U, Bergström C, van Steenberghe D. Survival of the Brånemark implant in partially edentulous jaws: a 10-year prospective multicenter study. Int J Oral Maxillofac Implants. 1999. 14:639–645.24. Skalak R. Biomechanical considerations in osseointegrated prostheses. J Prosthet Dent. 1983. 49:843–848.25. Davis DM, Rimrott R, Zarb GA. Studies on frameworks for osseointegrated prostheses: Part 2. The effect of adding acrylic resin or porcelain to form the occlusal superstructure. Int J Oral Maxillofac Implants. 1988. 3:275–280.26. Gracis SE, Nicholls JI, Chalupnik JD, Yuodelis RA. Shock absorbing behavior of five restorative materials used on implants. Int J Prosthodont. 1991. 4:282–291.27. Cibirka RM, Razzoog ME, Lang BR, Stohler CS. Determining the force absorption quotient for restorative materials used in implant occlusal surfaces. J Prosthet Dent. 1992. 67:361–364.28. Hobkirk JA, Psarros KJ. The influence of occlusal surface material on peak masticatory forces using osseointegrated implant-supported prostheses. Int J Oral Maxillofac Implants. 1992. 7:345–352.29. Sertgöz A. Finite element analysis study of the effect of superstructure material on stress distribution in an implant-supported fixed prosthesis. Int J Prosthodont. 1997. 10:19–27.30. Brunski JB, Puleo DA, Nanci A. Biomaterials and biomechanics of oral and maxillofacial implants: current status and future developments. Int J Oral Maxillofac Implants. 2000. 15:15–46.31. Glantz PO, Rangert B, Svensson A, Stafford GD, Arnvidarson B, Randow K, Lindén U, Hultén J. On clinical loading of osseointegrated implants. A methodological and clinical study. Clin Oral Implants Res. 1993. 4:99–105.32. Smedberg JI, Nilner K, Rangert B, Svensson SA, Glantz SA. On the influence of superstructure connection on implant preload: a methodological and clinical study. Clin Oral Implants Res. 1996. 7:55–63.33. Keaveny TM, Guo XE, Wachtel EF, McMahon TA, Hayes WC. Trabecular bone exhibits fully linear elastic behavior and yields at low strains. J Biomech. 1994. 27:1127–1136.34. Heckmann SM, Karl M, Wichmann MG, Winter W, Graef F, Taylor TD. Cement fixation and screw retention: parameters of passive fit. An in vitro study of three-unit implant-supported fixed partial dentures. Clin Oral Implants Res. 2004. 15:466–473.35. Karl M, Winter W, Taylor TD, Heckmann SM. In vitro study on passive fit in implant-supported 5-unit fixed partial dentures. Int J Oral Maxillofac Implants. 2004. 19:30–37.36. Curtis DA, Curtis TA, Wagnild GW, Finzen FC. Incidence of various classes of removable partial dentures. J Prosthet Dent. 1992. 67:664–667.37. Helkimo E, Carlsson GE, Helkimo M. Bite force and state of dentition. Acta Odontol Scand. 1977. 35:297–303.38. van Eijden TM. Three-dimensional analyses of human bite-force magnitude and moment. Arch Oral Biol. 1991. 36:535–539.39. Gibbs CH, Mahan PE, Mauderli A, Lundeen HC, Walsh EK. Limits of human bite strength. J Prosthet Dent. 1986. 56:226–229.40. Haraldson T, Karlsson U, Carlsson GE. Bite force and oral function in complete denture wearers. J Oral Rehabil. 1979. 6:41–48.41. Haraldson T, Carlsson GE, Ingervall B. Functional state, bite force and postural muscle activity in patients with osseointegrated oral implant bridges. Acta Odontol Scand. 1979. 37:195–206.42. Mericske-Stern R, Zarb GA. In vivo measurements of some functional aspects with mandibular fixed prostheses supported by implants. Clin Oral Implants Res. 1996. 7:153–161.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Implant Surgery for Fixed Implant-supported Prostheses in the Edentulous Mandible: A Case Report
- Occlusion for implant-supported fixed dental prostheses in partially edentulous patients: a literature review and current concepts
- Analysis of implant strain value exerted using different screw tightening protocols in screw-retained 3-unit prostheses
- Implant-assisted removable partial denture restoration in small number of residual teeth in mandible: A case report
- Complete mouth rehabilitation with fixed implant-supported prosthesis using temporary denture and dental CAD-CAM