Endocrinol Metab.
2013 Sep;28(3):231-235. 10.3803/EnM.2013.28.3.231.
Delayed Surgery for Parathyroid Adenoma Misdiagnosed as a Thyroid Nodule and Treated with Radiofrequency Ablation
- Affiliations
-
- 1Department of Internal Medicine, Gyeongsang National University School of Medicine, Jinju, Korea. taesikjung@gmail.com
- 2Department of Nuclear Medicine, Gyeongsang National University School of Medicine, Jinju, Korea.
- 3Institute of Health Sciences, Gyeongsang National University School of Medicine, Jinju, Korea.
- KMID: 1973829
- DOI: http://doi.org/10.3803/EnM.2013.28.3.231
Abstract
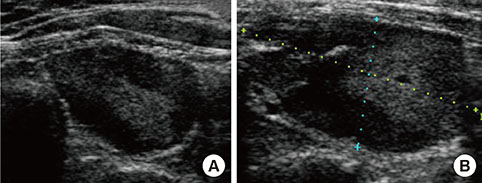
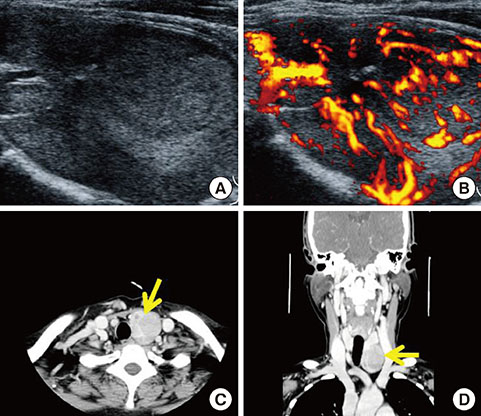
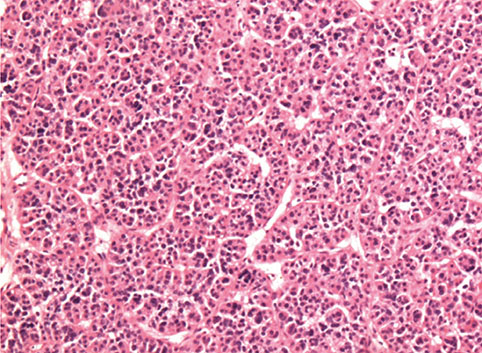
- Primary hyperparathyroidism occurs as a result of isolated parathyroid adenoma in 80% to 85% of all cases. A 99mtechnetium (99mTc) sestamibi scan or neck ultrasonography is used to localize the neoplasm prior to surgical intervention. A 53-year-old female was referred for the exclusion of metabolic bone disease. She presented with low back pain that had persisted for the past 6 months and elevated serum alkaline phosphatase (1,253 IU/L). Four years previously, she had been diagnosed at a local hospital with a 2.3-cm thyroid nodule, which was determined to be pathologically benign. Radiofrequency ablation was performed at the same hospital because the nodule was still growing during the follow-up period 2 years before the visit to our hospital, and the procedure was unsuccessful in reducing the size of the nodule. The results of the laboratory tests in our hospital were as follows: serum calcium, 14.6 mg/dL; phosphorus, 3.5 mg/dL; and intact parathyroid hormone (iPTH), 1,911 pg/mL. Neck ultrasonography and 99mTc sestamibi scan detected a 5-cm parathyroid neoplasm in the left lower lobe of the patient's thyroid; left parathyroidectomy was performed. This case indicated that thyroid ultrasonographers and pathologists need to be experienced enough to differentiate a parathyroid neoplasm from a thyroid nodule; 99mTc sestamibi scan, serum calcium, and iPTH levels can help to establish the diagnosis of parathyroid neoplasm.
MeSH Terms
-
Alkaline Phosphatase
Bone Diseases, Metabolic
Calcium
Female
Follow-Up Studies
Humans
Hyperparathyroidism, Primary
Low Back Pain
Middle Aged
Neck
Parathyroid Hormone
Parathyroid Neoplasms
Parathyroidectomy
Phosphorus
Technetium Tc 99m Sestamibi
Thyroid Gland
Thyroid Nodule
Alkaline Phosphatase
Calcium
Parathyroid Hormone
Phosphorus
Technetium Tc 99m Sestamibi
Figure
Cited by 1 articles
-
Brief Review of Articles in '
Endocrinology and Metabolism ' in 2013
Won-Young Lee
Endocrinol Metab. 2014;29(3):251-256. doi: 10.3803/EnM.2014.29.3.251.
Reference
-
1. Marcocci C, Cetani F. Clinical practice. Primary hyperparathyroidism. N Engl J Med. 2011; 365:2389–2397.2. Kwak JY, Kim EK, Moon HJ, Kim MJ, Ahn SS, Son EJ, Sohn YM. Parathyroid incidentalomas detected on routine ultrasound-directed fine-needle aspiration biopsy in patients referred for thyroid nodules and the role of parathyroid hormone analysis in the samples. Thyroid. 2009; 19:743–748.3. Lieu D. Cytopathologist-performed ultrasound-guided fineneedle aspiration of parathyroid lesions. Diagn Cytopathol. 2010; 38:327–332.4. Ha EJ, Baek JH, Lee JH. The efficacy and complications of radiofrequency ablation of thyroid nodules. Curr Opin Endocrinol Diabetes Obes. 2011; 18:310–314.5. Baek JH, Lee JH, Sung JY, Bae JI, Kim KT, Sim J, Baek SM, Kim YS, Shin JH, Park JS, Kim DW, Kim JH, Kim EK, Jung SL, Na DG. Korean Society of Thyroid Radiology. Complications encountered in the treatment of benign thyroid nodules with US-guided radiofrequency ablation: a multicenter study. Radiology. 2012; 262:335–342.6. Khati N, Adamson T, Johnson KS, Hill MC. Ultrasound of the thyroid and parathyroid glands. Ultrasound Q. 2003; 19:162–176.7. Nichols KJ, Tomas MB, Tronco GG, Rini JN, Kunjummen BD, Heller KS, Sznyter LA, Palestro CJ. Preoperative parathyroid scintigraphic lesion localization: accuracy of various types of readings. Radiology. 2008; 248:221–232.8. Giron J, Ouhayoun E, Dahan M, Berjaud J, Esquerre JP, Senac JP, Railhac JJ. Imaging of hyperparathyroidism: US, CT, MRI and MIBI scintigraphy. Eur J Radiol. 1996; 21:167–173.9. Krausz Y, Lebensart PD, Klein M, Weininger J, Blachar A, Chisin R, Shiloni E. Preoperative localization of parathyroid adenoma in patients with concomitant thyroid nodular disease. World J Surg. 2000; 24:1573–1578.10. Abraham D, Sharma PK, Bentz J, Gault PM, Neumayer L, McClain DA. Utility of ultrasound-guided fine-needle aspiration of parathyroid adenomas for localization before minimally invasive parathyroidectomy. Endocr Pract. 2007; 13:333–337.11. Mansoor I, Zalles C, Zahid F, Gossage K, Levenson RM, Rimm DL. Fine-needle aspiration of follicular adenoma versus parathyroid adenoma: the utility of multispectral imaging in differentiating lesions with subtle cytomorphologic differences. Cancer. 2008; 114:22–26.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiofrequency Ablation of Benign Thyroid Nodule
- Effective and Safe Application of Radiofrequency Ablation for Benign Thyroid Nodules
- Ultrasound (US)-Guided Ablation of Thyroid Nodules
- Response: Inquiries Regarding “Delayed Cancer Diagnosis in Thyroid Nodules Initially Treated as Benign With Radiofrequency Ablation: Ultrasound Characteristics and Predictors for Cancer”
- Diagnosis of Parathyroid Adenoma Detected during Thyroid Ultrasound: The Role of Parathormone Measurement in Fine-Needle Aspiration Washout