Clin Exp Otorhinolaryngol.
2014 Sep;7(3):181-187. 10.3342/ceo.2014.7.3.181.
Invasive Fungal Sinusitis of the Sphenoid Sinus
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Hwasun, Korea. limsc@chonnam.ac.kr
- 2Research Institute of Medical Sciences, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Hwasun, Korea.
- 3Department of Infectious Disease, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Hwasun, Korea.
- KMID: 1973467
- DOI: http://doi.org/10.3342/ceo.2014.7.3.181
Abstract
OBJECTIVE
This study was conducted to present the clinical outcome of invasive fungal sinusitis of the sphenoid sinus and to analyze clinical factors influencing patient survival.
METHODS
A retrospective review of 12 cases of invasive fungal sphenoiditis was conducted.
RESULTS
Cases were divided into acute fulminant invasive fungal spheonoidits (n=4) and chronic invasive fungal sphenoiditis (n=8). The most common underlying disease was diabetes mellitus (n=9). The most common presenting symptoms and signs included visual disturbance (100%). Intracranial extension was observed in 8 patients. Endoscopic debridement and intravenous antifungals were given to all patients. Fatal aneurysmal rupture of the internal carotid artery occurred suddenly in two patients. The mortality rate was 100% for patients with acute fulminant invasive fungal sphenoiditis and 25% for patients with chronic invasive fungal sphenoiditis. In survival analysis, intracranial extension was evaluated as a statistically significant factor (P=0.027).
CONCLUSION
The survival rate of chronic invasive fungal sphenoiditis was 75%. However, the prognosis of acute fulminant invasive fungal sphenoiditis was extremely poor despite the application of aggressive treatment, thus, a high index of suspicion should be required and new diagnostic markers need to be developed for early diagnosis of invasive fungal sinusitis of the sphenoid sinus.
Keyword
MeSH Terms
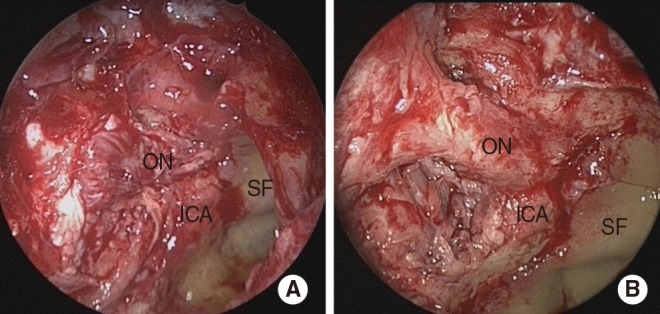
Figure
Reference
-
1. deShazo RD, O'Brien M, Chapin K, Soto-Aguilar M, Gardner L, Swain R. A new classification and diagnostic criteria for invasive fungal sinusitis. Arch Otolaryngol Head Neck Surg. 1997; 11. 123(11):1181–1188. PMID: 9366697.
Article2. deShazo RD, Chapin K, Swain RE. Fungal sinusitis. N Engl J Med. 1997; 7. 337(4):254–259. PMID: 9227932.
Article3. Ferguson BJ. Definitions of fungal rhinosinusitis. Otolaryngol Clin North Am. 2000; 4. 33(2):227–235. PMID: 10736401.
Article4. Rowe-Jones JM, Moore-Gillon V. Destructive noninvasive paranasal sinus aspergillosis: component of a spectrum of disease. J Otolaryngol. 1994; 4. 23(2):92–96. PMID: 8028079.5. Chopra H, Dua K, Bhatia S, Dua N, Mittal V. Invasive rhino-orbital fungal sinusitis following dental manipulation. Mycoses. 2009; 7. 52(4):368–371. PMID: 18705660.
Article6. Macedo DP, Neves RP, Fontan J, Souza-Motta CM, Lima D. A case of invasive rhinosinusitis by Fusarium verticillioides (Saccardo) Nirenberg in an apparently immunocompetent patient. Med Mycol. 2008; 8. 46(5):499–503. PMID: 18608897.7. Suryanarayan Rao S, Panda NK, Pragache G, Chakrabarti A, Saravanan K. Sinoorbital mucormycosis due to Apophysomyces elegans in immunocompetent individuals: an increasing trend. Am J Otolaryngol. 2006; Sep-Oct. 27(5):366–369. PMID: 16935188.8. Chopra H, Dua K, Malhotra V, Gupta RP, Puri H. Invasive fungal sinusitis of isolated sphenoid sinus in immunocompetent subjects. Mycoses. 2006; 1. 49(1):30–36. PMID: 16367816.
Article9. Chakrabarti A, Denning DW, Ferguson BJ, Ponikau J, Buzina W, Kita H, et al. Fungal rhinosinusitis: a categorization and definitional sche-ma addressing current controversies. Laryngoscope. 2009; 9. 119(9):1809–1818. PMID: 19544383.10. De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008; 6. 46(12):1813–1821. PMID: 18462102.
Article11. Baumann A, Zimmerli S, Hausler R, Caversaccio M. Invasive sphenoidal aspergillosis: successful treatment with sphenoidotomy and voriconazole. ORL J Otorhinolaryngol Relat Spec. 2007; 69(2):121–126. PMID: 17159376.
Article12. Gilony D, Talmi YP, Bedrin L, Ben-Shosan Y, Kronenberg J. The clinical behavior of isolated sphenoid sinusitis. Otolaryngol Head Neck Surg. 2007; 4. 136(4):610–615. PMID: 17418260.
Article13. An YH, Venkatraman G, DelGaudio JM. Isolated inflammatory sphenoid sinus disease: a revisitation of computed tomography indications based on presenting findings. Am J Rhinol. 2005; Nov-Dec. 19(6):627–632. PMID: 16402654.
Article14. Blitzer A, Lawson W, Meyers BR, Biller HF. Patient survival factors in paranasal sinus mucormycosis. Laryngoscope. 1980; 4. 90(4):635–648. PMID: 7359982.
Article15. Loftus BC. General principles of management of fungal infections of the head and neck. Otolaryngol Clin North Am. 1993; 12. 26(6):1115–1121. PMID: 8290284.
Article16. Aribandi M, McCoy VA, Bazan C 3rd. Imaging features of invasive and noninvasive fungal sinusitis: a review. Radiographics. 2007; Sep-Oct. 27(5):1283–1296. PMID: 17848691.
Article17. Groppo ER, El-Sayed IH, Aiken AH, Glastonbury CM. Computed tomography and magnetic resonance imaging characteristics of acute invasive fungal sinusitis. Arch Otolaryngol Head Neck Surg. 2011; 10. 137(10):1005–1010. PMID: 22006778.
Article18. Dhiwakar M, Thakar A, Bahadur S. Invasive sino-orbital aspergillosis: surgical decisions and dilemmas. J Laryngol Otol. 2003; 4. 117(4):280–285. PMID: 12816217.
Article19. Leventakos K, Lewis RE, Kontoyiannis DP. Fungal infections in leukemia patients: how do we prevent and treat them? Clin Infect Dis. 2010; 2. 50(3):405–415. PMID: 20047485.
Article20. Vallejo C, Barberán J. Empirical antifungal treatment: a valid alternative for invasive fungal infection. Rev Esp Quimioter. 2011; 9. 24(3):117–122. PMID: 21947092.21. Mainville N, Jordan DR. Orbital apergillosis treated with retrobulbar amphotericin B. Orbit. 2012; 2. 31(1):15–17. PMID: 22029690.22. Wakabayashi T, Oda H, Kinoshita N, Ogasawara A, Fujishiro Y, Kawanabe W. Retrobulbar amphotericin B injections for treatment of invasive sino-orbital aspergillosis. Jpn J Ophthalmol. 2007; Jul-Aug. 51(4):309–311. PMID: 17660997.
Article23. Segal E, Menhusen MJ, Shawn S. Hyperbaric oxygen in the treatment of invasive fungal infections: a single-center experience. Isr Med Assoc J. 2007; 5. 9(5):355–357. PMID: 17591371.24. Knipping S, Holzhausen HJ, Koesling S, Bloching M. Invasive aspergillosis of the paranasal sinuses and the skull base. Eur Arch Otorhinolaryngol. 2007; 10. 264(10):1163–1169. PMID: 17534639.
Article25. Choi HS, Choi JY, Yoon JS, Kim SJ, Lee SY. Clinical characteristics and prognosis of orbital invasive aspergillosis. Ophthal Plast Reconstr Surg. 2008; Nov-Dec. 24(6):454–459.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Three Cases of Fungal Sinusitis with Orbital Complication
- A Case of Fungal Sphenoid Sinusitis with Visual Loss
- A Case of Fungal Sphenoidal Sinusitis Involving Optic Nerve
- A Case of Optic Neuropathy Secondary to Sphenoid Sinus Aspergillosis
- A Case of Visual Loss Caused by Invasive Fungal Sinusitis of the Onodi Cell