J Korean Assoc Oral Maxillofac Surg.
2014 Apr;40(2):61-67. 10.5125/jkaoms.2014.40.2.61.
Comparison of the reproducibility of results of a new peri-implantitis assessment system (implant success index) with the Misch classification
- Affiliations
-
- 1Department of Periodontics, Dental School, Shahid Beheshti University of Medical Sciences, Tehran, Iran. Kadkhodazadehmahdi@yahoo.ir
- 2Department of Community Oral Health (COH) Clinical Epidemiology, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
- 3Private Practice, Isfahan, Iran.
- KMID: 1960956
- DOI: http://doi.org/10.5125/jkaoms.2014.40.2.61
Abstract
OBJECTIVES
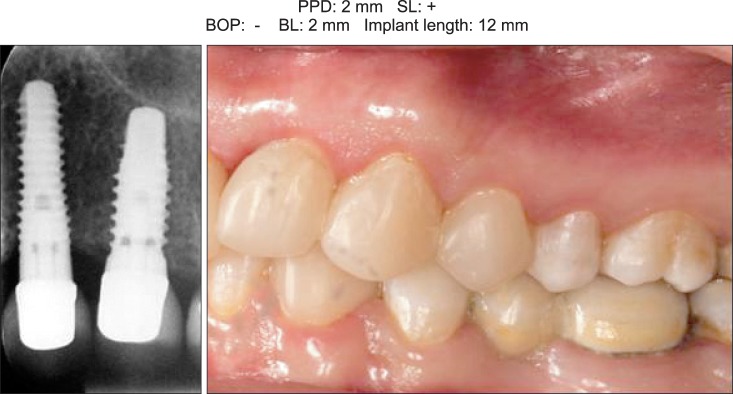
The present study was conducted to determine the reproducibility of peri-implant tissue assessment using the new implant success index (ISI) in comparison with the Misch classification.
MATERIALS AND METHODS
In this descriptive study, 22 cases of peri-implant soft tissue with different conditions were selected, and color slides were prepared from them. The slides were shown to periodontists, maxillofacial surgeons, prosthodontists and general dentists, and these professionals were asked to score the images according to the Misch classification and ISI. The intra- and inter-observer reproducibility scores of the viewers were assessed and reported using kappa and weighted kappa (WK) tests.
RESULTS
Inter-observer reproducibility of the ISI technique between the prosthodontists-periodontists (WK=0.85), prosthodontists-maxillofacial surgeons (WK=0.86) and periodontists-maxillofacial surgeons (WK=0.9) was better than that between general dentists and other specialists. In the two groups of general dentists and maxillofacial surgeons, ISI was more reproducible than the Misch classification system (WK=0.99 versus WK non-calculable, WK=1 and WK=0.86). The intra-observer reproducibility of both methods was equally excellent among periodontists (WK=1). For prosthodontists, the WK was not calculable via any of the methods.
CONCLUSION
The intra-observer reproducibility of both the ISI and Misch classification techniques depends on the specialty and expertise of the clinician. Although ISI has more classes, it also has higher reproducibility than simpler classifications due to its ability to provide more detail.
Keyword
Figure
Cited by 1 articles
-
Assessment of interleukin-1beta and interleukin-6 in the crevicular fluid around healthy implants, implants with peri-implantitis, and healthy teeth: a cross-sectional study
Siamak Yaghobee, Afshin Khorsand, Amir Alireza Rasouli Ghohroudi, Khashayar Sanjari, Mahdi Kadkhodazadeh
J Korean Assoc Oral Maxillofac Surg. 2014;40(5):220-224. doi: 10.5125/jkaoms.2014.40.5.220.
Reference
-
1. Albrektsson T, Isidor F. In : Lang NP, Karring T, editors. Consensus report: implant therapy. Proceeding of the 1st European Workshop on Periodontology; Berlin: Quintessence;1994. p. 365–369.2. Le Guéhennec L, Soueidan A, Layrolle P, Amouriq Y. Surface treatments of titanium dental implants for rapid osseointegration. Dent Mater. 2007; 23:844–854. PMID: 16904738.
Article3. Davarpanah M, Martinez H, Etienne D, Zabalegui I, Mattout P, Chiche F, et al. A prospective multicenter evaluation of 1,583 3i implants: 1- to 5-year data. Int J Oral Maxillofac Implants. 2002; 17:820–828. PMID: 12507242.4. Astrand P, Engquist B, Dahlgren S, Gröndahl K, Engquist E, Feldmann H. Astra Tech and Brånemark system implants: a 5-year prospective study of marginal bone reactions. Clin Oral Implants Res. 2004; 15:413–420. PMID: 15248875.5. Nelson K, Semper W, Hildebrand D, Ozyuvaci H. A retrospective analysis of sandblasted, acid-etched implants with reduced healing times with an observation period of up to 5 years. Int J Oral Maxillofac Implants. 2008; 23:726–732. PMID: 18807571.6. Tonetti MS. Risk factors for osseodisintegration. Periodontol 2000. 1998; 17:55–62. PMID: 10337313.
Article7. Berglundh T, Lindhe J, Marinello C, Ericsson I, Liljenberg B. Soft tissue reaction to de novo plaque formation on implants and teeth. An experimental study in the dog. Clin Oral Implants Res. 1992; 3:1–8. PMID: 1420721.
Article8. Ericsson I, Berglundh T, Marinello C, Liljenberg B, Lindhe J. Long-standing plaque and gingivitis at implants and teeth in the dog. Clin Oral Implants Res. 1992; 3:99–103. PMID: 1290796.
Article9. Zitzmann NU, Berglundh T. Definition and prevalence of peri-implant diseases. J Clin Periodontol. 2008; 35(8 Suppl):286–291. PMID: 18724856.
Article10. Leonhardt A, Dahlén G, Renvert S. Five-year clinical, microbiological, and radiological outcome following treatment of peri-implantitis in man. J Periodontol. 2003; 74:1415–1422. PMID: 14653386.
Article11. Behneke A, Behneke N, d'Hoedt B, Wagner W. Hard and soft tissue reactions to ITI screw implants: 3-year longitudinal results of a prospective study. Int J Oral Maxillofac Implants. 1997; 12:749–757. PMID: 9425755.12. Jovanovic SA. The management of peri-implant breakdown around functioning osseointegrated dental implants. J Periodontol. 1993; 64(11 Suppl):1176–1183. PMID: 8295108.
Article13. Roos-Jansåker AM, Lindahl C, Renvert H, Renvert S. Nine- to fourteen-year follow-up of implant treatment. Part II: presence of peri-implant lesions. J Clin Periodontol. 2006; 33:290–295. PMID: 16553638.
Article14. Offenbacher S. Periodontal diseases: pathogenesis. Ann Periodontol. 1996; 1:821–878. PMID: 9118282.
Article15. Albandar JM. Global risk factors and risk indicators for periodontal diseases. Periodontol 2000. 2002; 29:177–206. PMID: 12102708.
Article16. Mombelli A, Lang NP. The diagnosis and treatment of peri-implantitis. Periodontol 2000. 1998; 17:63–76. PMID: 10337314.
Article17. Brägger U, Aeschlimann S, Bürgin W, Hämmerle CH, Lang NP. Biological and technical complications and failures with fixed partial dentures (FPD) on implants and teeth after four to five years of function. Clin Oral Implants Res. 2001; 12:26–34. PMID: 11168268.
Article18. Kadkhodazadeh M, Amid R. Evaluation of peri-implant tissue health using a scoring system. JIACD. 2012; 4:51–57.19. Misch CE, Perel ML, Wang HL, Sammartino G, Galindo-Moreno P, Trisi P, et al. Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent. 2008; 17:5–15. PMID: 18332753.
Article20. Rothman KJ, Greenland S, Lash TL. Modern epidemiology. 3rd ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins;2008. p. 307–308.21. Kadkhodazadeh M, Esfahrood ZR, Amid R, Zarnegarnia P. Comparison of the acceptability of a new scoring system with Misch's classification for dental implant success determination. J Long Term Eff Med Implants. 2012; 22:85–93. PMID: 23016792.
Article22. Murphy EA. The logic of medicine. 2nd ed. Baltimore: Johns Hopkins University Press;1997. p. 119–136.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Implant success rates in full-arch rehabilitations supported by upright and tilted implants: a retrospective investigation with up to five years of follow-up
- Risk factors of peri-implantitis: a narrative review
- Peri-implant disease: what we know and what we need to know
- Unusual bone regeneration following resective surgery and decontamination of peri-implantitis: a 6-year follow-up
- Retrospective analysis of keratinized tissue augmentation using a xenogeneic collagen matrix for resolving peri-implant mucositis and peri-implantitis