J Korean Endocr Soc.
2007 Dec;22(6):470-474. 10.3803/jkes.2007.22.6.470.
A Case of Primary Hyperparathyroidism Associated with Gall-bladder Stone and Chronic Cholecystitis
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University Wonju College of Medicine, Korea.
- 2Department of Pathology, Yonsei University Wonju College of Medicine, Korea.
- KMID: 1958914
- DOI: http://doi.org/10.3803/jkes.2007.22.6.470
Abstract
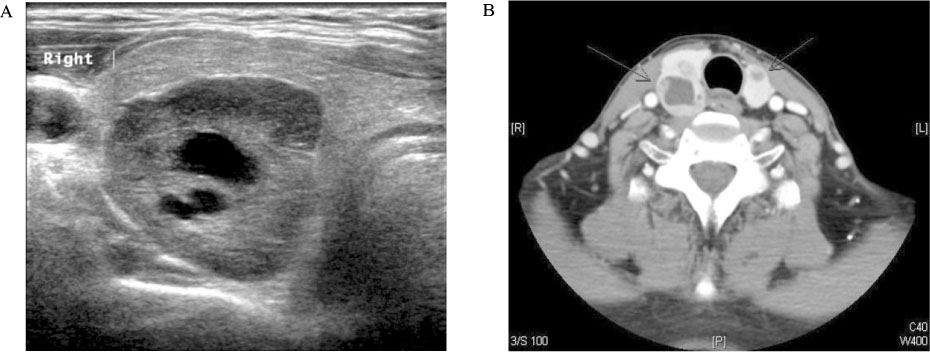
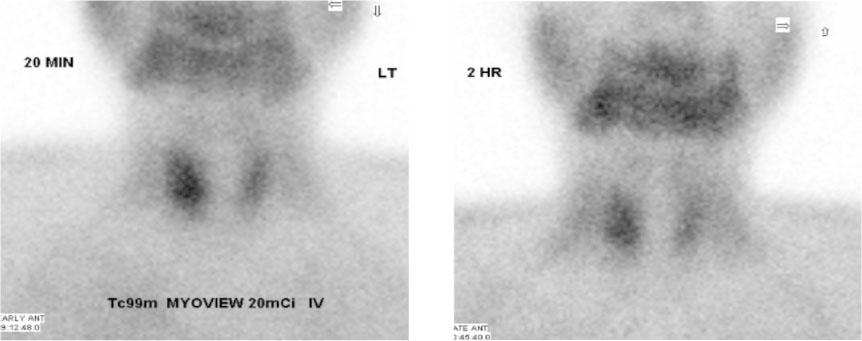
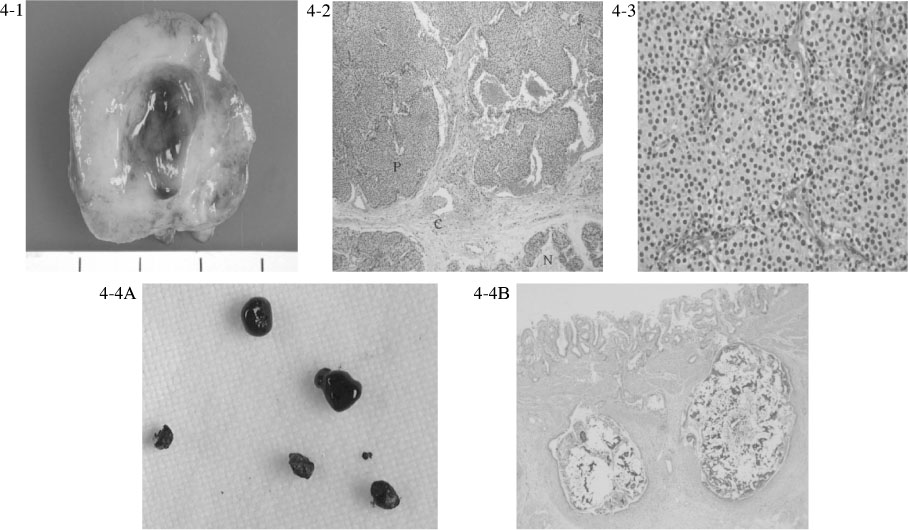
- Primary hyperparathyroidism is caused mainly by a parathyroid adenoma or hyperplasia, and is characterized by hypercalcemia and hypophosphatemia induced by an increased level of parathyroid hormone (PTH). Patients with primary hyperparathyroidism are usually asymptomatic and the disease is most often detected incidentally. However, patients can present with symptoms of renal stones, peptic ulcer disease, muscle weakness, depression, constipation, and pancreatitis. In addition, it has been reported that choletithiasis can be combined with primary hyperparathyroidism. We report a case of a 49-year-old man with primary hyperparathyroidism accompanied with chronic cholecystitis caused by a gallbladder (GB) stone. The chief complaint was nausea, poor oral intake, abdominal pain, and weight loss. Abdominal sonography was performed and chronic cholecystitis with a GB stone was diagnosed. The serum calcium level was 18.5 mg/dL and the intact parathyroid hormone level was 1,777 pg/mL. A parathyroid mass was detected by neck-computed tomography, neck ultrasonography and a (99m)Tc-Tetrofosmin parathyroid scan. The parathyroid mass was removed and the mass was confirmed as a parathyroid adenoma. Cholecystectomy was performed and the diagnosis of chronic cholecystitis was confirmed. After the surgical procedure, the symptoms improved and the calcium level was normalized.
MeSH Terms
-
Abdominal Pain
Calcium
Cholecystectomy
Cholecystitis*
Cholelithiasis
Constipation
Depression
Diagnosis
Gallbladder
Humans
Hypercalcemia
Hyperparathyroidism, Primary*
Hyperplasia
Hypophosphatemia
Middle Aged
Muscle Weakness
Nausea
Neck
Pancreatitis
Parathyroid Hormone
Parathyroid Neoplasms
Peptic Ulcer
Ultrasonography
Weight Loss
Calcium
Parathyroid Hormone
Figure
Reference
-
1. Park BM, Chu JB. A case of primary hyperparathyroidism. J Korean Surg Soc. 1963. 5:391–395.2. Chung HK, Kim DY, Woo JT, Kim SW, Yang IM, Kim JW, Kim YS, Kim KW, Choi YK. Review of clinical characteristics of primary hyperparathyroidism. J Kor Soc Endocrinol. 1992. 7:234–242.3. Broulik PD, Haas T, Adámek S. Analysis of 645 patients with primary hyperparathyroidism with special references to cholelithiasis. Intern Med. 2005. 44:917–921.4. Park JM, Kim GL, Pyun HY, Cho SR, Yeo JK, Park KY, Hur JW, Lee IK. The incidence and causes of hypercalcemia in a hospital population. J Kor Soc Endocrinol. 1993. 8:72–77.5. Lee GM, Noh DY, Choe KJ, Youn YK, Oh Sk. Primary hyperparathyroidism. J Korean Surg Soc. 2001. 60:273–280.6. Lee JB, Lee ES, Bae CW, Koo BW. Symptomatic primary hyperparathyroidism. J Korean Surg Soc. 1998. 55:794–799.7. Lee SW, Park H, Shin JM, Lee YM, Park JH, Koh YW, Mok JO, Kwon KW. Clinical analysis of parathyroid adenoma with primary hyperparathyroidism. Korean J Otolaryngol. 2006. 49:72–78.8. Christensson T, Hellstrom K, Wengle B, Alveryd A, Wikland B. Prevalence of hypercalcemia in a health screening in Stockholm. Acta Med Scand. 1976. 200:131–137.9. Potts JT, Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL. Harrison's Principles of Internal Medicine. 2005. 16th Ed. New York: McGraw-Hill;2249–2263.10. Selle JG, Altemeier WA, Fullen WD, Goldsmith RE. Cholelithiasis in hyperparathyroidism: a neglected manifestation. Arch Surg. 1972. 105:369–374.11. Mok LL, Nickols GA, Thompson JC, Cooper CW. Parathyroid hormone as a smooth muscle relaxant. Endocr Rev. 1989. 10:420–436.12. Layer P, Hotz J, Sinewe S, Goebell H. Bile secretion in acute and chronic hypercalcemia in the cat. Dig Dis Sci. 1986. 31:188–192.13. Ahrendt SA, Ahrendt GM, Pitt HA, Moore EW, Lillemoe KD. Hypercalcemia decreases bile flow and increases biliary calcium in the prairie dog. Surgery. 1995. 117:435–442.14. Kim GH, Ok CM, Kim BJ, Joo HJ, Song CS, Song GA, Cho M, Yang US. A clinical review of gallstone diseases in Koreans. Kor J Gastroenterol. 1997. 29:352–361.15. Kim MH, Ohrr HC, Chung JB, Kim CD, Kang JK, Koh MS, Kim NJ, Kim DG, Kim SK, Kim YS, Kim YT, Kim JH, Roh IH, Kim YI, Park SH, Seol SY, Shim CS, Yang US, Yeo HS, Rew JS, Yoon YB, Lee SK, Chung MK, Choi SC. The epidemiologic study on Korean gallstone disease a nationwide cooperative study. Kor J Gastroenterol. 1998. 32:635–647.16. Choi KN, Kim JM. A clinical review of gallbladder and biliary tract stones. J Korean Surg Soc. 1998. 55:405–413.17. Park SJ, Kim SH, Park YC, Kim YT, Yun YB, Park YH. Clinical and epidemiological analysis of a 20-Year experience of surgically treated gallstone patients. Kor J Gastroenterol. 2003. 42:415–422.18. Carey MC, Cahalane MJ. Whither biliary sludge? Gastroenterology. 1988. 95:508–523.