Ann Surg Treat Res.
2014 Aug;87(2):66-71. 10.4174/astr.2014.87.2.66.
Rationale and surgical technique of laparoscopic left lateral sectionectomy using endoscopic staples
- Affiliations
-
- 1Department of Surgery, Yeungnam University Medical Center, Daegu, Korea. ssyun@med.yu.ac.kr
- KMID: 1882833
- DOI: http://doi.org/10.4174/astr.2014.87.2.66
Abstract
- PURPOSE
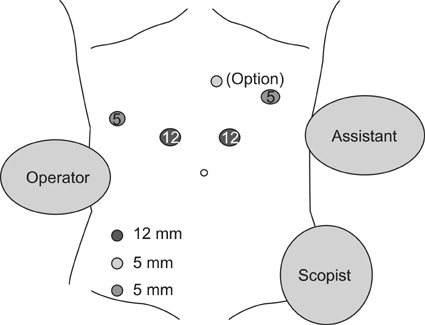
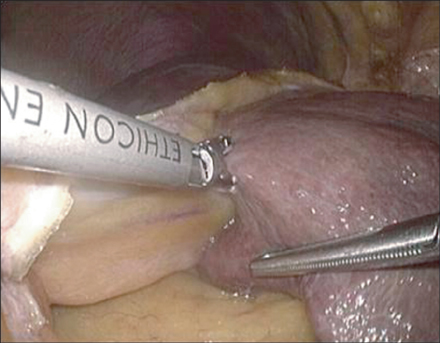
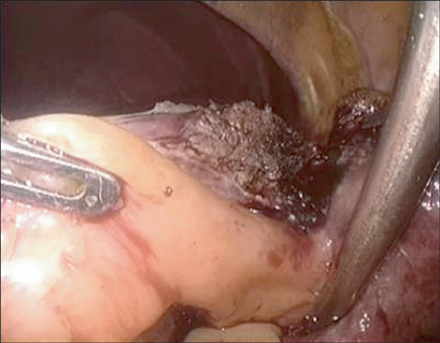
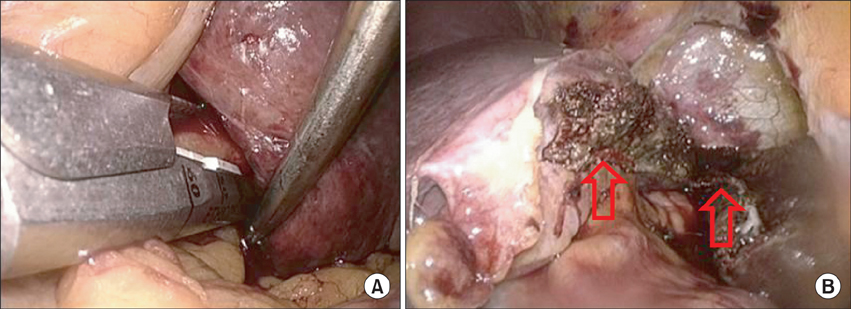
Laparoscopic left lateral sectionectomy (LLLS) has been widely accepted due to benefits of minimally invasive surgery. Some surgeons prefer to isolate glissonian pedicles to segments II and III and to control individual pedicles with surgical clips, whereas opt like to control glissonian pedicles simultaneously using endoscopic stapling devices. The aim of this study was to find the rationale of LLLS using endoscopic staples.
METHODS
We retrospectively analyzed and compared the clinical outcomes (operation time, drainage length, transfusion, hospital stay, and complication rate) of 35 patients that underwent LLLS between April 2004 and February 2012. Patients were dichotomized by surgical technique based on whether glissonian pedicles were isolated and controlled (the individual group, n = 21) or controlled using endoscopic staples at once (the batch group, n = 14).
RESULTS
Mean operation time was 265.3 +/- 21.3 minutes (mean +/- standard deviation) in the individual group and 170 +/- 22.9 minutes in the batch group. Operation time in the batch group was significantly shorter than the individual group (P = 0.007). Mean drainage length was 4.8 +/- 1.6 and 2.6 +/- 1.5 days in the individual and the batch group. There was significantly shorter in the batch group, also (P = 0.006). No transfusion was required in the batch group, but 4 patients in the individual group needed transfusion. Mean hospital stay was 10.7 +/- 1.1 and 9.4 +/- 0.8 days in the individual and the batch groups (P = 0.460). There were no significant complications or mortality in both groups.
CONCLUSION
LLLS using endoscopic staples (batch group) was found to be an easier and safer technique without morbidity or mortality.
Keyword
MeSH Terms
Figure
Reference
-
1. Abu Hilal M, Pearce NW. Laparoscopic left lateral liver sectionectomy: a safe, efficient, reproducible technique. Dig Surg. 2008; 25:305–308.2. Chang S, Laurent A, Tayar C, Karoui M, Cherqui D. Laparoscopy as a routine approach for left lateral sectionectomy. Br J Surg. 2007; 94:58–63.3. Gumbs AA, Gayet B, Gagner M. Laparoscopic liver resection: when to use the laparoscopic stapler device. HPB (Oxford). 2008; 10:296–303.4. Buell JF, Cherqui D, Geller DA, O'Rourke N, Iannitti D, Dagher I, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg. 2009; 250:825–830.5. Nguyen KT, Geller DA. Laparoscopic liver resection: current update. Surg Clin North Am. 2010; 90:749–760.6. Belli G, Gayet B, Han HS, Wakabayashi G, Kim KH, Cannon R, et al. Laparoscopic left hemihepatectomy a consideration for acceptance as standard of care. Surg Endosc. 2013; 27:2721–2726.7. Yamamoto M, Katagiri S, Ariizumi S, Kotera Y, Takahashi Y. Glissonean pedicle transection method for liver surgery (with video). J Hepatobiliary Pancreat Sci. 2012; 19:3–8.8. Lesurtel M, Cherqui D, Laurent A, Tayar C, Fagniez PL. Laparoscopic versus open left lateral hepatic lobectomy: a case-control study. J Am Coll Surg. 2003; 196:236–242.9. Wang X, Li J, Wang H, Luo Y, Ji W, Duan W, et al. Validation of the laparoscopically stapled approach as a standard technique for left lateral segment liver resection. World J Surg. 2013; 37:806–811.10. Hasegawa Y, Nitta H, Sasaki A, Takahara T, Ito N, Fujita T, et al. Laparoscopic left lateral sectionectomy as a training procedure for surgeons learning laparoscopic hepatectomy. J Hepatobiliary Pancreat Sci. 2013; 20:525–530.11. Linden BC, Humar A, Sielaff TD. Laparoscopic stapled left lateral segment liver resection: technique and results. J Gastrointest Surg. 2003; 7:777–782.12. Khan AZ, Prasad KR, Lodge JP, Toogood GJ. Laparoscopic left lateral sectionectomy: surgical technique and our results from Leeds. J Laparoendosc Adv Surg Tech A. 2009; 19:29–32.13. Azagra JS, Goergen M, Gilbart E, Jacobs D. Laparoscopic anatomical (hepatic) left lateral segmentectomy-technical aspects. Surg Endosc. 1996; 10:758–761.14. Cho A, Okazumi S, Yoshinaga Y, Ishikawa Y, Ryu M, Ochiai T. Relationship between left biliary duct system and left portal vein: evaluation with three-dimensional portocholangiography. Radiology. 2003; 228:246–250.15. Cho A, Okazumi S, Miyazawa Y, Makino H, Miura F, Ohira G, et al. Proposal for a reclassification of liver based anatomy on portal ramifications. Am J Surg. 2005; 189:195–199.16. Broelsch CE, Whitington PF, Emond JC, Heffron TG, Thistlethwaite JR, Stevens L, et al. Liver transplantation in children from living related donors. Surgical techniques and results. Ann Surg. 1991; 214:428–437.17. Shirouzu Y, Ohya Y, Hayashida S, Yoshii T, Asonuma K, Inomata Y. Reduction of left-lateral segment from living donors for liver transplantation in infants weighing less than 7 kg: technical aspects and outcome. Pediatr Transplant. 2010; 14:709–714.18. Kaneko H, Otsuka Y, Takagi S, Tsuchiya M, Tamura A, Shiba T. Hepatic resection using stapling devices. Am J Surg. 2004; 187:280–284.19. Kim SJ, Jung HK, Lee DS, Yun SS, Kim HJ. The comparison of oncologic and clinical outcomes of laparoscopic liver resection for hepatocellular carcinoma. Ann Surg Treat Res. 2014; 86:61–67.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Solo Reduced Port Laparoscopic Left Lateral Sectionectomy
- Outcomes of Laparoscopic Left Lateral Sectionectomy vs. Open Left Lateral Sectionectomy: Single Center Experience
- Early outcomes of single-port robotic left lateral sectionectomy in patients with hepatic tumor
- Pure laparoscopic versus open left lateral sectionectomy for hepatocellular carcinoma: A propensity score matching analysis
- Is left lateral sectionectomy of the liver without operative site drainage safe and effective?