J Cerebrovasc Endovasc Neurosurg.
2015 Jun;17(2):108-112. 10.7461/jcen.2015.17.2.108.
Endovascular Treatment in Ruptured Middle Cerebral Artery Dissection Preservation of Arterial Continuity
- Affiliations
-
- 1Department of Neurosurgery, Kimpo Woori Hospital, Kimpo, Korea.
- 2Department of Neurosurgery, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea. contacting@lycos.co.kr
- KMID: 1879342
- DOI: http://doi.org/10.7461/jcen.2015.17.2.108
Abstract
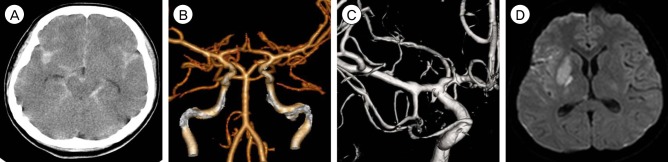
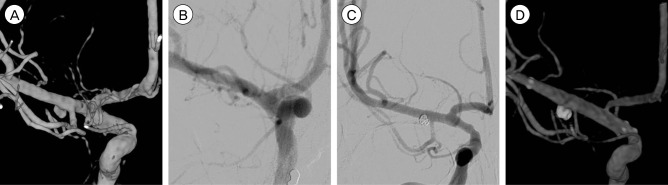
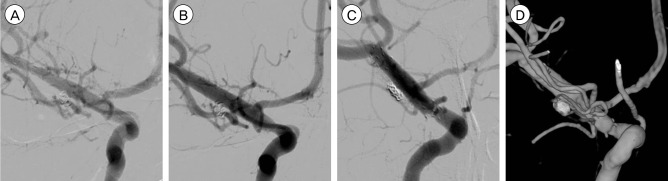
- Rupture of spontaneous dissecting aneurysms of the middle cerebral artery (MCA) is rare and its etiology remains obscure, although the risk of rebleeding is greater than with saccular aneurysms. Most reports concerning the treatment of a ruptured dissecting aneurysm of the anterior circulation involve surgical trapping or wrapping. Here, we report on a case of an MCA dissecting rupture treated with endovascular procedures. A 22-year-old female presented with sudden stuporous mental change following severe headache and left side hemiparesis. A computed tomography scan showed a diffuse subarachnoid hemorrhage and diffusion MR showed diffusion restriction at the right putamen and internal capsule. A 3-hour follow-up digital subtraction angiography (DSA) showed a dissecting aneurysm, which was not seen on an initial DSA. A stent assisted coil embolization was performed and double stents were applied to achieve flow diversion effects. A small remnant area of the dissecting aneurysm had disappeared at 60-day and was not observed on 12-month follow-up DSA.
Keyword
MeSH Terms
Figure
Reference
-
1. Chan RS, Mak CH, Wong AK, Chan KY, Leung KM. Use of the pipeline embolization device to treat recently ruptured dissecting cerebral aneurysms. Interv Neuroradiol. 2014; Jul-Aug. 20(4):436–441. PMID: 25207906.
Article2. Chuang MJ, Lu CH, Cheng MH. Management of middle cerebral artery dissecting aneurysm. Asian J Surg. 2012; 1. 35(1):42–48. PMID: 22726563.
Article3. Fischer S, Perez MA, Kurre W, Albes G, Bazner H, Henkes H. Pipeline embolization device for the treatment of intra- and extracranial fusiform and dissecting aneurysms: initial experience and long-term follow-up. Neurosurgery. 2014; 10. 75(4):364–374. discussion 374PMID: 24871140.4. Friedman AH, Drake CG. Subarachnoid hemorrhage from intracranial dissecting aneurysm. J Neurosurg. 1984; 2. 60(2):325–334. PMID: 6693960.
Article5. Gong D, Yan B, Dowling R, Mitchell P. Successful treatment of growing basilar artery dissecting aneurysm by pipeline flow diversion embolization device. J Stroke Cerebrovasc Dis. 2014; 7. 23(6):1713–1716. PMID: 24389375.
Article6. Hosoda K, Fujita S, Kawaguchi T, Shose Y, Yonezawa K, Shirakuni T, et al. Spontaneous dissecting aneurysms of the basilar artery presenting with a subarachnoid hemorrhage. Report of two cases. J Neurosurg. 1991; 10. 75(4):628–633. PMID: 1885981.7. Kawaguchi S, Sakaki T, Tsunoda S, Morimoto T, Hoshida T, Kawai S, et al. Management of dissecting aneurysms of the posterior circulation. Acta Neurochir (Wien). 994; 3. 131(1-2):26–31. PMID: 7709782.
Article8. Kim YW, Yoo SH, Kim SR, Kim SD, Park IS, Baik MW. Dissecting aneurysm at the A1 segment of the anterior cerebral artery manifesting as subarachnoid hemorrhage: two case reports. Korean J Cerebrovasc Surg. 2005; 12. 7(4):324–328.9. Kitanaka C, Sasaki T, Eguchi T, Teraoka A, Nakane M, Hoya K. Intracranial vertebral artery dissections: clinical, radiological features, and surgical considerations. Neurosurgery. 1994; 4. 34(4):620–626. discussion 266-7PMID: 8008158.10. Kunze S, Schiefer W. Angiographic demonstration of a dissecting aneurysm of the middle cerebral artery. Neuroradiology. 1971; 9. 2(4):201–206. PMID: 5164128.
Article11. Kurata A, Ohmomo T, Miyasaka Y, Fujii K, Kan S, Kitahara T. Coil embolization for the treatment of ruptured dissecting vertebral aneurysms. AJNR Am J Neuroradiol. 2001; 1. 22(1):11–18. PMID: 11158881.12. Kurino M, Yoshioka S, Ushio Y. Spontaneous dissecting aneurysms of anterior and middle cerebral artery associated with brain infarction: a case report and review of the literature. Surg Neurol. 2002; 6. 57(6):428–436. discussion 436-8PMID: 12176212.13. Manabe H, Hatayama T, Hasegawa S, Islam SM, Suzuki S. Coil embolisation for ruptured vertebral artery dissection distal to the origin of the posterior inferior cerebellar artery. Neuroradiology. 2000; 5. 42(5):384–387. PMID: 10872163.
Article14. Manabe H, Ohkuma H, Fujita S, Suzuki S. Coil embolization of ruptured vertebral dissection in acute stage with interlocking detachable coils. Surg Neurol. 1997; 5. 47(5):476–480. PMID: 9131033.
Article15. Ohkuma H, Suzuki S, Shimamura N, Nakano T. Dissecting aneurysms of the middle cerebral artery: neuroradiological and clinical features. Neuroradiology. 2003; 3. 45(3):143–148. PMID: 12684715.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment for subarachnoid hemorrhage due to ruptured posterior cerebral arterial dolichoectasia with aortic arch anomaly
- Coil Embolization for Distal Middle Cerebral Artery Aneurysm
- Spontaneous Anterior Cerebral Artery Dissection Presenting with Simultaneous Subarachnoid Hemorrhage and Cerebral Infarction in a Patient with Multiple Extracranial Arterial Dissections
- Successful Endovascular Treatment of Ruptured Superior Cerebellar Artery Aneurysm Associated with Moyamoya Disease : A Case Report and Review of the Literature
- Y-Stenting Endovascular Treatment for Ruptured Intracranial Aneurysms : A Single-Institution Experience in Korea