Obstet Gynecol Sci.
2014 Jul;57(4):325-329. 10.5468/ogs.2014.57.4.325.
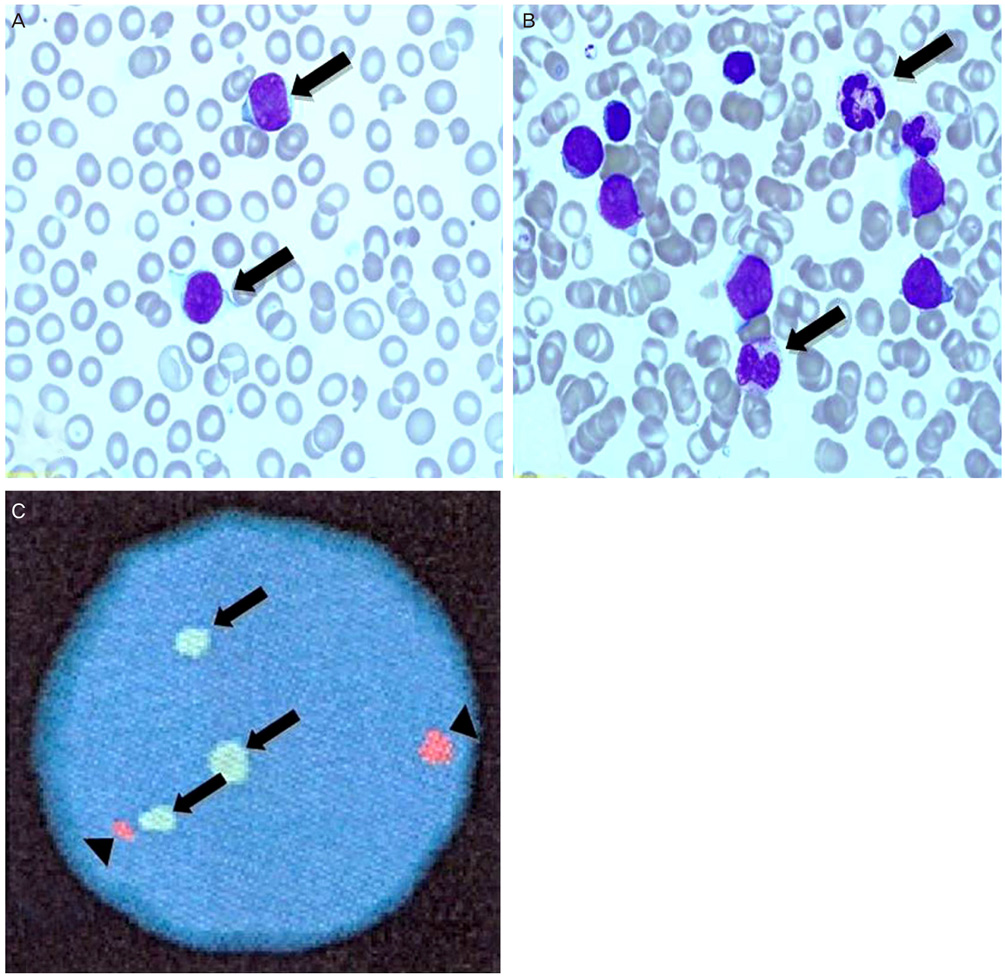
Congenital leukemia of fetus with acquired AML1 gene duplication
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Pusan National University School of Medicine, Busan, Korea. ksch0127@naver.com
- 2Department of Pediatrics, Pusan National University School of Medicine, Busan, Korea.
- 3Department of Laboratory Medicine, Pusan National University School of Medicine, Busan, Korea.
- KMID: 1841546
- DOI: http://doi.org/10.5468/ogs.2014.57.4.325
Abstract
- Congenital leukemia is very rare, and its prevalence according to recently published papers is from 1 to 5 per million live births. This can be often diagnosed in postpartum throughout bone marrow biopsy, showing abnormal proliferation of immature blasts and granulocytic precursors. Hepatosplenomegaly is the most common feature which is found during perinatal examinations, that diagnosing is difficult during perinatal period. Hepatosplenomegaly can occur not only in congenital leukemia but in many other cases such as infection which is the most common cause. In other words, congenital leukemia is the one of the rare causes of hepatosplenomegaly. However, this case shows the fetus with the features of hepatosplenomegaly during perinatal period and being diagnosed as congenital leukemia associated with acquired AML1 gene duplication in postpartum through bone marrow biopsy. Due to its rare instance, we are to describe the case with a review of literatures.
Keyword
Figure
Reference
-
1. Bader JL, Miller RW. US cancer incidence and mortality in the first year of life. Am J Dis Child. 1979; 133:157–159.2. Badhe PB, Sane SY. Congenital leukemia: organ involvement in six autopsy cases. J Postgrad Med. 1992; 38:127–129.3. Bargotra R, Suri J, Gupta Y. Congenital leukemia. JK Sci. 2010; 12:201–202.4. Prakash KP, Rau AT, Bhat ST, Rau AR. Congenital leukemia: a diagnostic dilemma. Indian J Med Paediatr Oncol. 2008; 29:41–43.5. Bronshtein M, Blazer S, Zimmer EZ. The gastrointestinal tract and abdominal wall. In : Callen PW, editor. Ultrasonography in obstetrics and gynecology. 5th ed. Philadelphia: Saunders Elsevier;2008. p. 615–623.6. Vintzileos AM, Neckles S, Campbell WA, Andreoli JW Jr, Kaplan BM, Nochimson DJ. Fetal liver ultrasound measurements during normal pregnancy. Obstet Gynecol. 1985; 66:477–480.7. Schmidt W, Yarkoni S, Jeanty P, Grannum P, Hobbins JC. Sonographic measurements of the fetal spleen: clinical implications. J Ultrasound Med. 1985; 4:667–672.8. Choi JH, Lee HB, Park CW, Lee CH. A case of congenital leukemia cutis. Ann Dermatol. 2009; 21:66–70.9. Harewood L, Robinson H, Harris R, Al-Obaidi MJ, Jalali GR, Martineau M, et al. Amplification of AML1 on a duplicated chromosome 21 in acute lymphoblastic leukemia: a study of 20 cases. Leukemia. 2003; 17:547–553.10. Sande JE, Arceci RJ, Lampkin BC. Congenital and neonatal leukemia. Semin Perinatol. 1999; 23:274–285.11. Nathan DG, Oski FA. Congenital leukemia. In : Nathan DG, Oski FA, editors. Hematology of infancy and childhood. 3rd ed. Philadelphia: Saunders;1987. p. 1052–1053.12. Van der Linden MH, Creemers S, Pieters R. Diagnosis and management of neonatal leukaemia. Semin Fetal Neonatal Med. 2012; 17:192–195.13. Bresters D, Reus AC, Veerman AJ, van Wering ER, van der Does-van den Berg A, Kaspers GJ. Congenital leukaemia: the Dutch experience and review of the literature. Br J Haematol. 2002; 117:513–524.14. Isaacs H Jr. Fetal and neonatal leukemia. J Pediatr Hematol Oncol. 2003; 25:348–361.15. Grundy RG, Martinez A, Kempski H, Malone M, Atherton D. Spontaneous remission of congenital leukemia: a case for conservative treatment. J Pediatr Hematol Oncol. 2000; 22:252–255.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of biphenotypic acute leukemia with expression of the AML1-ETO gene rearrangement
- Detection of Residual Leukemia with Reverse Transcription-polymerase Chain Reaction from Patients with AML1/ETO Positive Acute Myeloid Leukemia in Remission
- AML1/ETO Fusion Gene Expression and Clinical Characteristics of Adult Acute Myelogenous Leukemia
- TEL/AML1 Fusion Transcripts in Childhood B-Lineage Acute Lymphoblastic Leukemia
- Molecular Cytogenetic Analysis of Gene Rearrangements in Childhood Acute Lymphoblastic Leukemia