Korean J Urogenit Tract Infect Inflamm.
2015 Apr;10(1):25-30. 10.14777/kjutii.2015.10.1.25.
Effectiveness of Topical Ofloxacin Ointment for Genitourinary Post-Operative Patients with Urinary Catheterization
- Affiliations
-
- 1Department of Urology, National Police Hospital, Seoul, Korea. drmsk@korea.com
- 2Department of Laboratory Medicine, National Police Hospital, Seoul, Korea.
- KMID: 1839385
- DOI: http://doi.org/10.14777/kjutii.2015.10.1.25
Abstract
- PURPOSE
Catheter associated urinary tract infection and discomfort is common in patients with an indwelling urinary catheter. We investigated the effectiveness of prophylactic topical antibiotic ointment for genitourinary post-operative patients with a urinary catheter.
MATERIALS AND METHODS
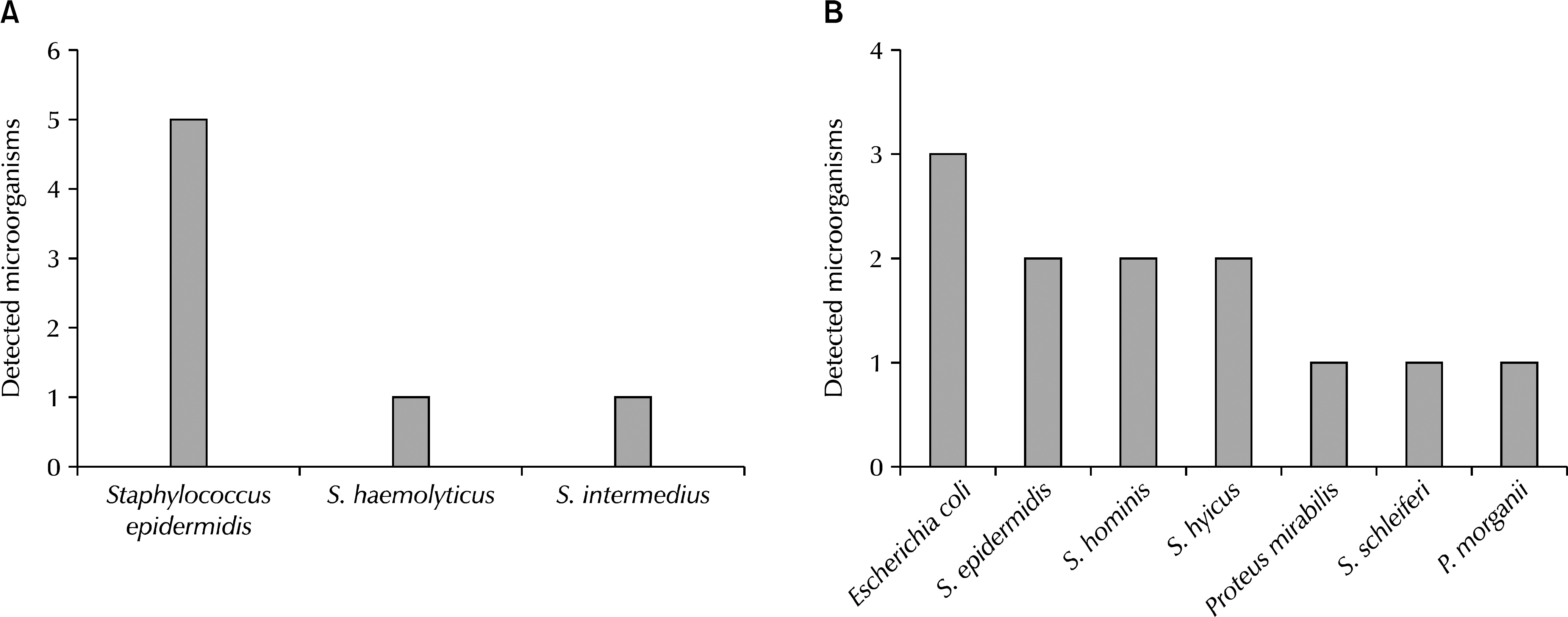
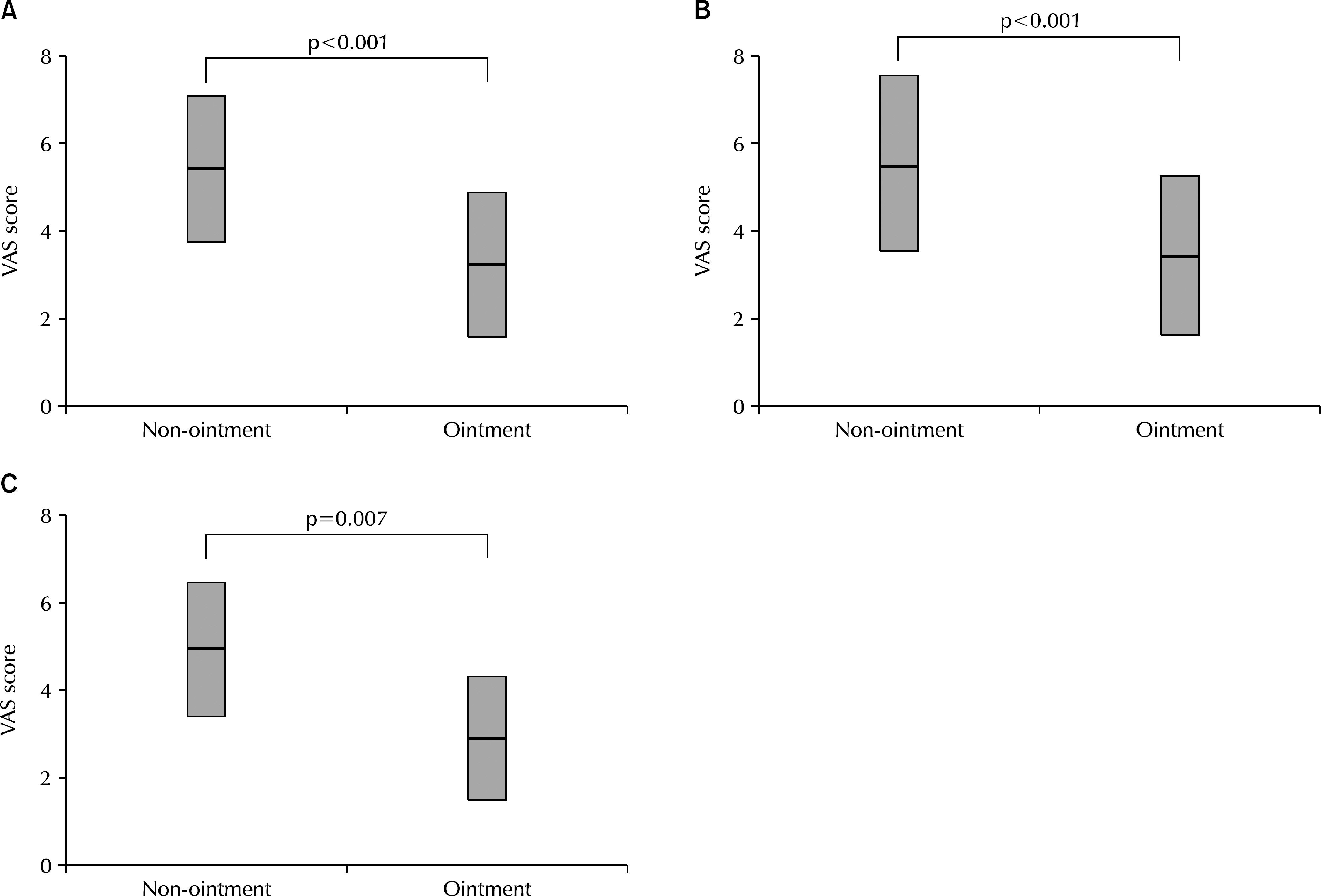
We investigated 112 inpatients between March 2013 and October 2013, who had an indwelling urinary catheter > or =24 hours after a genitourinary operation in our institution from medical records. Among 112 patients, 59 patients applied ofloxacin ointment to urethral meatus around the indwelling catheter twice a day (ointment group: 52.7%) and 53 patients did not (non-ointment group: 47.3%). All patients were examined by urine analysis and urine culture before the operation, urethral sweep culture after catheter removal, and severity of pain was recorded as visual analogue scale (VAS) score while having an indwelling urinary catheter.
RESULTS
Mean duration of urinary catheter of both groups did not differ statistically (3.08+/-2.19 day, 2.91+/-2.25 day). Patients with pyuria detected at pre-operative urinalysis were 22.1% vs. 15.1%, pre-operative urine culture positive were 6.8% vs. 9.4%, urethra meatal culture positive after urethral catheter removal were 16.9% vs. 13.2%, respectively, and all results showed no significant differences between two groups. VAS scores of the ointment group (3.52+/-1.66) while having an indwelling urinary catheter were significantly lower than those of the non-ointment group (5.61+/-1.75) (p<0.001).
CONCLUSIONS
Application of topical antibiotic ointment for genitourinary post-operative patients with urinary catheter had no benefit in reducing growth of urethral microorganisms, but it may decrease pain from an indwelling urinary catheter.
Keyword
MeSH Terms
Figure
Reference
-
1. Yim SH, Ha US, Sohn DW, Lee SJ, Han CH, Lee CB, et al. Treatment and prevention of catheter-associated urinary tract infections. Korean J Urogenit Tract Infect Inflamm. 2009; 4:159–69.2. Yoo JY, Shim BS, Yoon H. Preliminary study on protective effect of urovaxomⓇ in the longterm urinary catheterized patients. Korean J Urogenit Tract Infect Inflamm. 2008; 3:95–8.3. Warren JW, Tenney JH, Hoopes JM, Muncie HL, Anthony WC. A prospective microbiologic study of bacteriuria in patients with chronic indwelling urethral catheters. J Infect Dis. 1982; 146:719–23.
Article4. Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC, et al. Infectious Diseases Society of America. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010; 50:625–63.
Article5. Yoon H. European and Asian guidelines on management and prevention of catheter-associated urinary tract infections. Korean J Urogenit Tract Infect Inflamm. 2008; 3:137–47.6. Yang SO. Catheter-associated urinary tract infection. Korean J Urogenit Tract Infect Inflamm. 2013; 8:73–82.
Article7. Classen DC, Larsen RA, Burke JP, Stevens LE. Prevention of catheter-associated bacteriuria: clinical trial of methods to block three known pathways of infection. Am J Infect Control. 1991; 19:136–42.8. Burke JP, Garibaldi RA, Britt MR, Jacobson JA, Conti M, Alling DW. Prevention of catheter-associated urinary tract infections. Efficacy of daily meatal care regimens. Am J Med. 1981; 70:655–8.9. Tenke P, Kovacs B, Bjerklund Johansen TE, Matsumoto T, Tambyah PA, Naber KG. European and Asian guidelines on management and prevention of catheter-associated urinary tract infections. Int J Antimicrob Agents. 2008; 31(Suppl 1):S68–78.
Article10. Platt R, Polk BF, Murdock B, Rosner B. Risk factors for nosocomial urinary tract infection. Am J Epidemiol. 1986; 124:977–85.
Article11. Warren JW, Bakke A, Desgranchamps F, Johnson JR, Kumon H, Shah J, et al. Catheter-associated bacteriuria and the role of biomaterial in prevention. Naber KG, Pechere JC, Kumazawa J, Khoury S, Gerberding IL, Schaeffer AJ, editors. Nosocomial and health care associated infections in urology. Plymouth: Health Publications Ltd;2001. p. 153–76.12. Sedor J, Mulholland SG. Hospital-acquired urinary tract infections associated with the indwelling catheter. Urol Clin North Am. 1999; 26:821–8.
Article13. Stamm WE, Hooton TM, Johnson JR, Johnson C, Stapleton A, Roberts PL, et al. Urinary tract infections: from pathogenesis to treatment. J Infect Dis. 1989; 159:400–6.
Article14. Warren JW. Catheter-associated urinary tract infections. Int J Antimicrob Agents. 2001; 17:299–303.
Article15. Steward DK, Wood GL, Cohen RL, Smith JW, Mackowiak PA. Failure of the urinalysis and quantitative urine culture in diagnosing symptomatic urinary tract infections in patients with longterm urinary catheters. Am J Infect Control. 1985; 13:154–60.
Article16. Tambyah PA, Maki DG. Catheter-associated urinary tract infection is rarely symptomatic: a prospective study of 1,497 catheterized patients. Arch Intern Med. 2000; 160:678–82.
Article17. Bergqvist D, Bronnestam R, Hedelin H, Stahl A. The relevance of urinary sampling methods in patients with indwelling Foley catheters. Br J Urol. 1980; 52:92–5.
Article18. Ibrahim AI. Hospital acquired pre-prostatectomy bacteriuria: risk factors and implications. East Afr Med J. 1996; 73:107–10.19. Grabe M, Hellsten S. Bacteriuria, a risk factor in men with bladder outlet obstruction. Kass EM, Svanborg E, editors. Host parasite interaction in urinary tract infection. Göteborg: University of Göteborg;1986. p. 303–6.20. Sullivan NM, Sutter VL, Mims MM, Marsh VH, Finegold SM. Clinical aspects of bacteremia after manipulation of the genitourinary tract. J Infect Dis. 1973; 127:49–55.
Article21. Bregenzer T, Frei R, Widmer AF, Seiler W, Probst W, Mattarelli G, et al. Low risk of bacteremia during catheter replacement in patients with longterm urinary catheters. Arch Intern Med. 1997; 157:521–5.
Article22. Tambyah PA, Oon J. Catheter-associated urinary tract infection. Curr Opin Infect Dis. 2012; 25:365–70.
Article23. Patel AR, Jones JS, Babineau D. Lidocaine 2% gel versus plain lubricating gel for pain reduction during flexible cystoscopy: a metaanalysis of prospective, randomized, controlled trials. J Urol. 2008; 179:986–90.
Article24. Ho KJ, Thompson TJ, O'Brien A, Young MR, McCleane G. Lignocaine gel: does it cause urethral pain rather than prevent it? Eur Urol. 2003; 43:194–6.
Article25. Siderias J, Gaudio F, Singer AJ. Comparison of topical anesthetics and lubricants prior to urethral catheterization in males: a randomized controlled trial. Acad Emerg Med. 2004; 11:703–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Periocular Allergic Contact Dermatitis Associated with the Use of Ofloxacin Ophthalmic Ointment: A Case Report
- Effect of Ointment Containing Epithelial Growth Factor Compared with Antibacterial Ointment in Avulsive Laceration
- Ocular Penetration of Topical Ofloxacin in Rabbit Eye with Amniotic Membrane Transplantation
- Mupirocin Ointment Prevents Early Post-Tympanostomy Tube Otorrhea: A Preliminary Study
- Allergic Contact Dermatits due to Cambison Ophthalmic Ointment