Korean Circ J.
2011 Aug;41(8):440-446. 10.4070/kcj.2011.41.8.440.
Relation Between High-Sensitivity C-Reactive Protein and Coronary Plaque Components in Patients With Acute Coronary Syndrome: Virtual Histology-Intravascular Ultrasound Analysis
- Affiliations
-
- 1Heart Center of Chonnam National University Hospital, Chonnam National University Research Institute of Medical Sciences, Gwangju, Korea. myungho@chollian.net
- KMID: 1826350
- DOI: http://doi.org/10.4070/kcj.2011.41.8.440
Abstract
- BACKGROUND AND OBJECTIVES
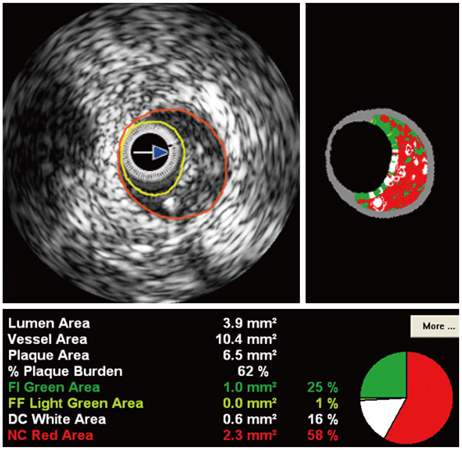
We used virtual histology-intravascular ultrasound (VH-IVUS) to evaluate the relationship between high-sensitivity C-reactive protein (hs-CRP) levels and plaque components in 279 acute coronary syndrome (ACS) patients.
SUBJECTS AND METHODS
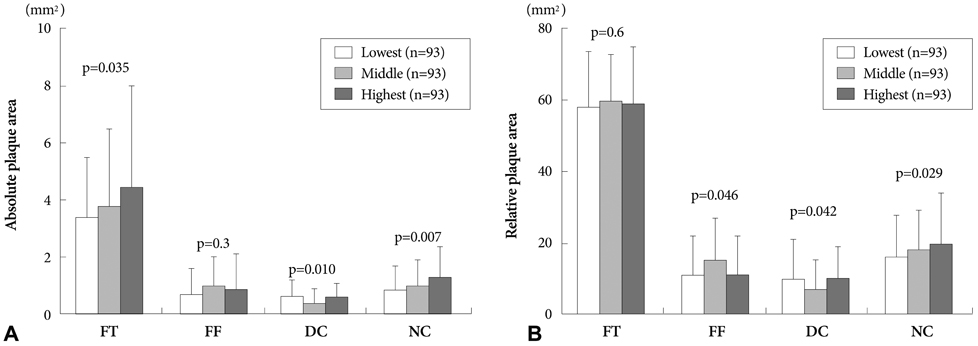
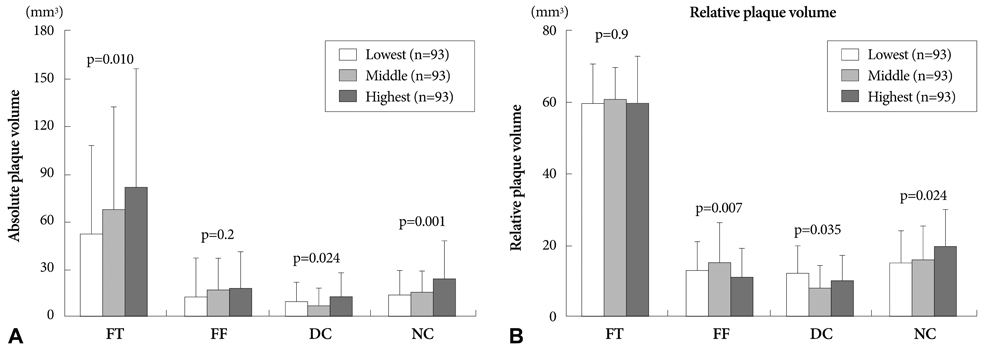
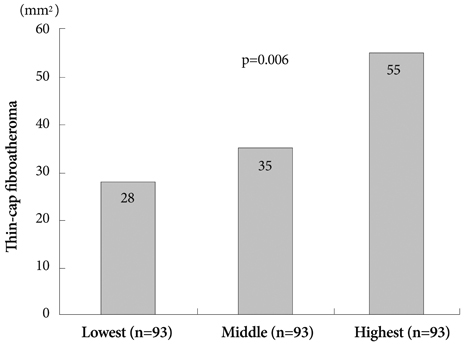
We divided patients into three groups according to their hs-CRP levels {lowest tertile <0.07 mg/dL (n=93), middle tertile > or =0.07, <0.4 mg/dL (n=93), and highest tertile > or =0.4 mg/dL (n=93)}. Thin-cap fibroatheroma (TCFA) was defined as focal, necrotic core (NC)-rich (> or =10% of the cross-sectional area) plaques in contact with the lumen in a plaque burden > or =40%.
RESULTS
The highest tertile group was mostly diabetics (20%, 27%, 40%, p=0.009), and had the greatest plaque plus media volume (163+/-139/mm3 vs. 201+/-155/mm3 vs. 232+/-176/mm3, p=0.013). The highest tertile group had the greatest absolute and % NC volumes (13.6+/-15.1 mm3 vs. 14.8+/-14.2 mm3 vs. 23.7+/-24.3 mm3, p<0.001, and 14.9+/-8.7% vs. 16.0+/-8.7% vs. 19.5+/-10.2%, p=0.024, respectively). The culprit lesion TCFA was observed most frequently in the highest tertile group (28% vs. 35% vs. 55%, p=0.006). By multivariable analysis, absolute NC volume was an independent predictor of hs-CRP elevation {odds ratio (OR); 1.03, 95% confidence interval (CI)=1.06-1.21, p=0.004}, and hs-CRP was an independent predictor of TCFA (OR; 1.86, 95% CI=1.11-2.90, p=0.010).
CONCLUSION
VH-IVUS analysis has demonstrated that ACS patients with elevated hs-CRP have more vulnerable plaque component (NC-rich plaques and higher frequency of culprit lesion TCFA), compared with ACS patients with normal hs-CRP.
Keyword
MeSH Terms
Figure
Reference
-
1. Choi H, Cho DH, Shin HH, Park JB. Association of high sensitivity C-reactive protein with coronary heart disease prediction, but not with carotid atherosclerosis, in patients with hypertension. Circ J. 2004. 68:297–303.2. Nakanishi N, Shiraishi T, Wada M. C-reactive protein concentration is more strongly related to metabolic syndrome in women than in men: the Minoh Study. Circ J. 2005. 69:386–391.3. Ridker PM, Glynn RJ, Hennekens CH. C-reactive protein adds to the predictive value of total and HDL cholesterol in determining risk of first myocardial infarction. Circulation. 1998. 97:2007–2011.4. Morrow DA, Braunwald E. Future of biomarkers in acute coronary syndromes: moving toward a multimarker strategy. Circulation. 2003. 108:250–252.5. Pearson TA, Mensah GA, Alexander RW, et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003. 107:499–511.6. Sano T, Tanaka A, Namba M, et al. C-reactive protein and lesion morphology in patients with acute myocardial infarction. Circulation. 2003. 108:282–285.7. Hong MK, Mintz GS, Lee CW, et al. Comparison of coronary plaque rupture between stable angina and acute myocardial infarction: a three-vessel intravascular ultrasound study in 235 patients. Circulation. 2004. 110:928–933.8. Hur SH. Lesion characteristics in patients with acute coronary syndrome: a comparison with lesion in patients with stable angina by intravascular ultrasound. Korean Circ J. 2004. 34:548–557.9. Nian M, Lee P, Khaper N, Liu P. Inflammatory cytokines and postmyocardial infarction remodeling. Circ Res. 2004. 94:1543–1553.10. Tanaka A, Shimada K, Sano T, et al. Multiple plaque rupture and C-reactive protein in acute myocardial infarction. J Am Coll Cardiol. 2005. 45:1594–1599.11. Rodriguez-Granillo GA, García-García HM, Mc Fadden EP, et al. In vivo intravascular ultrasound-derived thin-cap fibroatheroma detection using ultrasound radiofrequency data analysis. J Am Coll Cardiol. 2005. 46:2038–2042.12. Bae JH, Kwon TG, Kim KH, Hyun DW, Kim KY, Kim DS. In-vivo coronary plaque composition in patients with acute coronary syndrome: a virtual histology intravascular ultrasound study. Korean Circ J. 2007. 37:437–442.13. Roberts WL, Moulton L, Law TC, et al. Evaluation of nine automated high-sensitivity C-reactive protein methods: implications for clinical and epidemiological applications. Part 2. Clin Chem. 2001. 47:418–425.14. Mintz GS, Nissen SE, Anderson WD, et al. American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, Measurement and Reporting of Intravascular Ultrasound Studies (IVUS): a report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2001. 37:1478–1492.15. Bae JH, Rihal CS, Lerman A. Tissue characterization of coronary plaques using intravascular ultrasound/virtual histology. Korean Circ J. 2006. 36:553–558.16. Blake GJ, Ridker PM. C-reactive protein and other inflammatory risk markers in acute coronary syndromes. J Am Coll Cardiol. 2003. 41:4 Suppl S. 37S–42S.17. James SK, Armstrong P, Barnathan E, et al. Troponin and C-reactive protein have different relations to subsequent mortality and myocardial infarction after acute coronary syndrome: a GUSTO-IV substudy. J Am Coll Cardiol. 2003. 41:916–924.18. van der Meer IM, de Maat MP, Bots ML, et al. Inflammatory mediators and cell adhesion molecules as indicators of severity of atherosclerosis: the Rotterdam Study. Arterioscler Thromb Vasc Biol. 2002. 22:838–842.19. Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002. 105:1135–1143.20. Jabs WJ, Theissing E, Nitschke M, et al. Local generation of C-reactive protein in diseased coronary artery venous bypass grafts and normal vascular tissue. Circulation. 2003. 108:1428–1431.21. Davies MJ, Thomas A. Thrombosis and acute coronary-artery lesions in sudden cardiac ischemic death. N Engl J Med. 1984. 310:1137–1140.22. Farb A, Burke AP, Tang AL, et al. Coronary plaque erosion without rupture into a lipid core: a frequent cause of coronary thrombosis in sudden coronary death. Circulation. 1996. 93:1354–1363.23. Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol. 2000. 20:1262–1275.24. Falk E, Shah PK, Fuster V. Coronary plaque disruption. Circulation. 1995. 92:657–671.25. Davies MJ, Richardson PD, Woolf N, Katz DR, Mann J. Risk of thrombosis in human atherosclerotic plaques: role of extracellular lipid, macrophage, and smooth muscle cell content. Br Heart J. 1993. 69:377–381.26. Buja LM, Willerson JT. Role of inflammation in coronary plaque disruption. Circulation. 1994. 89:503–505.27. Virmani R, Burke AP, Kolodgie FD, Farb A. Pathology of the thin-cap fibroatheroma: a type of vulnerable plaque. J Interv Cardiol. 2003. 16:267–272.28. Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. J Am Coll Cardiol. 2006. 47:8 Suppl. C13–C18.29. Burke AP, Tracy RP, Kolodgie F, et al. Elevated C-reactive protein values and atherosclerosis in sudden coronary death: association with different pathologies. Circulation. 2002. 105:2019–2023.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Differential Changes in Coronary Plaque Composition According to Plaque Stability Following Statin Initiation in Acute Coronary Syndrome: Classification and Analysis by Intravascular Ultrasound-Virtual Histology
- Relationship between Neutrophil-to-Lymphocyte Ratio and Plaque Components in Patients with Coronary Artery Disease: Virtual Histology Intravascular Ultrasound Analysis
- Relation between Anemia and Vulnerable Coronary Plaque Components in Patients with Acute Coronary Syndrome: Virtual Histology-Intravascular Ultrasound Analysis
- In-Vivo Coronary Plaque Composition in Patients with Acute Coronary Syndrome: A Virtual Histology Intravascular Ultrasound Study
- Comparison of Coronary Plaque Components between Non-Culprit Lesions in Patients with Acute Coronary Syndrome and Target Lesions in Patients with Stable Angina: Virtual Histology-Intravascular Ultrasound Analysis