J Gynecol Oncol.
2014 Jan;25(1):58-63. 10.3802/jgo.2014.25.1.58.
Decreased ARID1A expression is correlated with chemoresistance in epithelial ovarian cancer
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Hirosaki University Graduate School of Medicine, Hirosaki, Japan. yokoyama@cc.hirosaki-u.ac.jp
- KMID: 1811189
- DOI: http://doi.org/10.3802/jgo.2014.25.1.58
Abstract
OBJECTIVE
Loss of ARID1A is related to oncogenic transformation of ovarian clear cell adenocarcinoma. The present study was conducted in epithelial ovarian cancer of all tissue types to investigate whether an increased or decreased expression level of ARID1A can be a prognostic factor for ovarian cancer or can influence the sensitivity to anticancer drugs.
METHODS
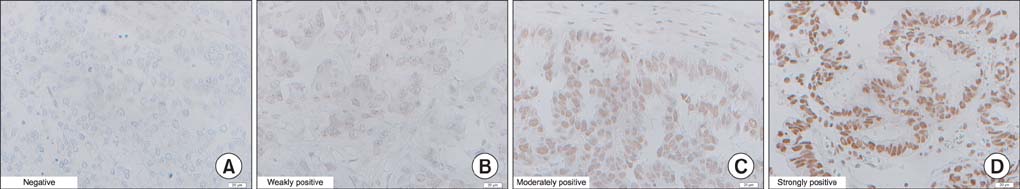
The expression level of ARID1A was investigated in 111 patients with epithelial ovarian cancer who received initial treatment at the Hirosaki University Hospital between 2006 and 2011. The expression level of ARID1A was immunohistochemically graded using staining scores, which were calculated by multiplying the staining intensity of the nuclei by the stain-positive area.
RESULTS
The level of ARID1A was significantly lower in clear cell adenocarcinoma than in other histologic types. Among the patients with stage III, IV cancer (n=46), the level of ARID1A was significantly lower (p=0.026) in patients who did not achieve complete response (CR; n=12) than in patients who achieved CR (n=34). The level of ARID1A was relatively lower (p=0.07) in patients who relapsed after achieving CR (n=21) than in patients who did not relapse (n=13). When the staining score of 0 was defined as ARID1A-negative and other staining scores were defined as ARID1A-positive, there was significant difference in progression-free survival between ARID1A-negative (n=11) and ARID1A-positive (n=35) patients in stage III, IV disease.
CONCLUSION
The result suggests that decreased ARID1A expression is correlated with chemoresistance and may be a predictive factor for the risk of relapse of advanced cancer after achieving CR.
Keyword
Figure
Reference
-
1. Ozols RF, Bundy BN, Greer BE, Fowler JM, Clarke-Pearson D, Burger RA, et al. Phase III trial of carboplatin and paclitaxel compared with cisplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: a Gynecologic Oncology Group study. J Clin Oncol. 2003; 21:3194–3200.2. FIGO (International Federation of Gynecology and Obstetrics) 26th Annual Report on the Results of Treatment in Gynecological Cancer. Int J Gynaecol Obstet. 2006; 95:Suppl 1. S1–S257.3. Burger RA, Brady MF, Bookman MA, Fleming GF, Monk BJ, Huang H, et al. Incorporation of bevacizumab in the primary treatment of ovarian cancer. N Engl J Med. 2011; 365:2473–2483.4. Katsumata N, Yasuda M, Takahashi F, Isonishi S, Jobo T, Aoki D, et al. Dose-dense paclitaxel once a week in combination with carboplatin every 3 weeks for advanced ovarian cancer: a phase 3, open-label, randomised controlled trial. Lancet. 2009; 374:1331–1338.5. Armstrong DK, Bundy B, Wenzel L, Huang HQ, Baergen R, Lele S, et al. Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N Engl J Med. 2006; 354:34–43.6. Jones S, Wang TL, Shih IeM, Mao TL, Nakayama K, Roden R, et al. Frequent mutations of chromatin remodeling gene ARID1A in ovarian clear cell carcinoma. Science. 2010; 330:228–231.7. Wiegand KC, Shah SP, Al-Agha OM, Zhao Y, Tse K, Zeng T, et al. ARID1A mutations in endometriosis-associated ovarian carcinomas. N Engl J Med. 2010; 363:1532–1543.8. Hargreaves DC, Crabtree GR. ATP-dependent chromatin remodeling: genetics, genomics and mechanisms. Cell Res. 2011; 21:396–420.9. Maeda D, Mao TL, Fukayama M, Nakagawa S, Yano T, Taketani Y, et al. Clinicopathological Significance of Loss of ARID1A Immunoreactivity in Ovarian Clear Cell Carcinoma. Int J Mol Sci. 2010; 11:5120–5128.10. Yamamoto S, Tsuda H, Takano M, Tamai S, Matsubara O. PIK3CA mutations and loss of ARID1A protein expression are early events in the development of cystic ovarian clear cell adenocarcinoma. Virchows Arch. 2012; 460:77–87.11. Yamamoto S, Tsuda H, Takano M, Tamai S, Matsubara O. Loss of ARID1A protein expression occurs as an early event in ovarian clear-cell carcinoma development and frequently coexists with PIK3CA mutations. Mod Pathol. 2012; 25:615–624.12. Samartzis EP, Samartzis N, Noske A, Fedier A, Caduff R, Dedes KJ, et al. Loss of ARID1A/BAF250a-expression in endometriosis: a biomarker for risk of carcinogenic transformation? Mod Pathol. 2012; 25:885–892.13. Lowery WJ, Schildkraut JM, Akushevich L, Bentley R, Marks JR, Huntsman D, et al. Loss of ARID1A-associated protein expression is a frequent event in clear cell and endometrioid ovarian cancers. Int J Gynecol Cancer. 2012; 22:9–14.14. Ayhan A, Mao TL, Seckin T, Wu CH, Guan B, Ogawa H, et al. Loss of ARID1A expression is an early molecular event in tumor progression from ovarian endometriotic cyst to clear cell and endometrioid carcinoma. Int J Gynecol Cancer. 2012; 22:1310–1315.15. Wu CH, Mao TL, Vang R, Ayhan A, Wang TL, Kurman RJ, et al. Endocervical-type mucinous borderline tumors are related to endometrioid tumors based on mutation and loss of expression of ARID1A. Int J Gynecol Pathol. 2012; 31:297–303.16. Wiegand KC, Lee AF, Al-Agha OM, Chow C, Kalloger SE, Scott DW, et al. Loss of BAF250a (ARID1A) is frequent in high-grade endometrial carcinomas. J Pathol. 2011; 224:328–333.17. Guan B, Mao TL, Panuganti PK, Kuhn E, Kurman RJ, Maeda D, et al. Mutation and loss of expression of ARID1A in uterine low-grade endometrioid carcinoma. Am J Surg Pathol. 2011; 35:625–632.18. Katagiri A, Nakayama K, Rahman MT, Rahman M, Katagiri H, Nakayama N, et al. Loss of ARID1A expression is related to shorter progression-free survival and chemoresistance in ovarian clear cell carcinoma. Mod Pathol. 2012; 25:282–288.19. Umemoto M, Yokoyama Y, Sato S, Tsuchida S, Al-Mulla F, Saito Y. Carbonyl reductase as a significant predictor of survival and lymph node metastasis in epithelial ovarian cancer. Br J Cancer. 2001; 85:1032–1036.20. Schiff PB, Horwitz SB. Taxol stabilizes microtubules in mouse fibroblast cells. Proc Natl Acad Sci U S A. 1980; 77:1561–1565.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ovarian cancer risk score predicts chemo-response and outcome in epithelial ovarian carcinoma patients
- Prognostic Significance of ARID1A Expression Patterns Varies with Molecular Subtype in Advanced Gastric Cancer
- Chemoresistance in ovarian cancer: exploiting cancer stem cell metabolism
- Rb pathway alteration and E2F-1 expression in epithelial ovarian cancer
- Expression of p21WAF1/CIP1/SDI1 in Epithelial Ovarian Cancer ; Its Relationship with p53 Expression and Prognostic Factors