J Cerebrovasc Endovasc Neurosurg.
2012 Sep;14(3):164-169. 10.7461/jcen.2012.14.3.164.
Mechanical Thrombectomy Using a Solitaire Stent in Acute Ischemic Stroke; Initial Experience in 40 Patients
- Affiliations
-
- 1Department of Neurosurgery, School of Medicine, Chungnam National University, Daejeon, Korea. solesoul@daum.net
- KMID: 1808450
- DOI: http://doi.org/10.7461/jcen.2012.14.3.164
Abstract
OBJECTIVE
This study was conducted in order to demonstrate the initial experience of the Solitaire AB stent in mechanical intracranial thrombectomy.
METHODS
We conducted a retrospective review of 40 consecutive patients who underwent intra-arterial Solitaire AB stent thrombectomy for treatment of acute ischemic strokes between October 2010 and November 2011. Demographic, clinical, and radiological presentations and outcomes were studied.
RESULTS
Twenty six men and 14 women with a mean initial National Institutes of Health Stroke Scale (NIHSS) score of 14.1 (range, 8-26) and a mean age of 65.4 (range, 32-89) years were included in this study. Occlusion sites were as follows: internal carotid artery (n = 11), middle cerebral artery M1 (n = 22), M2 (n = 5), and basilar artery (n = 2). Successful revascularization was achieved in 36 (90%) patients. The mean NIHSS score was 11.6 (range, 1-23) at 24 hours after the procedure, and 42.5% of patients showed a modified Rankin scale score of < or = 2 at 90 days. New occlusion by migrated emboli was observed in one (2.5%) case. Post-procedural intracerebral hemorrhage occurred in only one case (2.5%), with an all-cause mortality of two (5%).
CONCLUSION
The Solitaire AB device is a relatively safe and effective tool for use in performance of mechanical thrombectomy in patients with acute ischemic stroke.
MeSH Terms
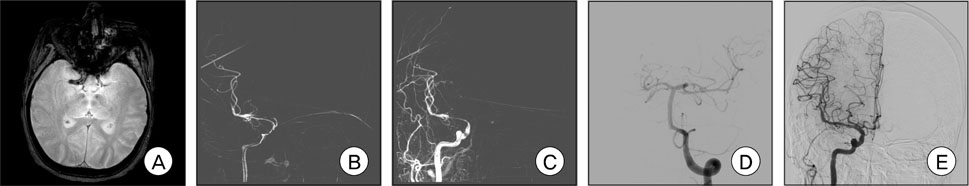
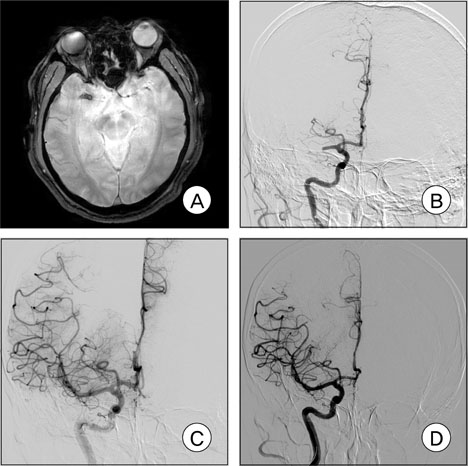
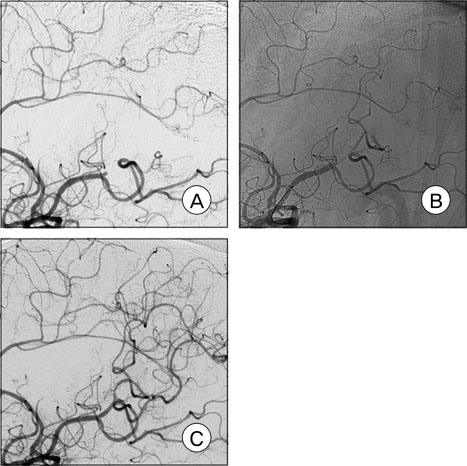
Figure
Cited by 1 articles
-
Angiographic and Clinical Factors Related with Good Functional Outcome after Mechanical Thrombectomy in Acute Cerebral Artery Occlusion
Jong Hyuk Park, Young Min Han, Kyeong Sool Jang, Wan Soo Yoon, Dong Kyu Jang, Sang Kyu Park
J Korean Neurosurg Soc. 2015;58(3):192-196. doi: 10.3340/jkns.2015.58.3.192.
Reference
-
1. Castano C, Dorado L, Guerrero C, Millan M, Gomis M, Perez de la Ossa N, et al. Mechanical thrombectomy with the Solitaire AB device in large artery occlusions of the anterior circulation: a pilot study. Stroke. 2010. 08. 41(8):1836–1840.2. Furlan A, Higashida R, Wechsler L, Gent M, Rowley H, Kase C, et al. Intra-arterial prourokinase for acute ischemic stroke: the PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA. 1999. 12. 282(21):2003–2011.3. Kelly ME, Furlan AJ, Fiorella D. Recanalization of an acute middle cerebral artery occlusion using a self-expanding, reconstrainable, intracranial microstent as a temporary endovascular bypass. Stroke. 2008. 06. 39(6):1770–1773.
Article4. Khatri P, Abruzzo T, Yeatts SD, Nichols C, Broderick JP, Tomsick TA. Good clinical outcome after ischemic stroke with successful revascularization is time-dependent. Neurology. 2009. 09. 73(13):1066–1072.
Article5. Krischek Ö, Miloslavski E, Fischer S, Shrivastava S, Henkes H. A comparison of functional and physical properties of self-expanding intracranial stents [Neuroform3, Wingspan, Solitaire, Leo(+), Enterprise]. Minim Invasive Neurosurg. 2011. 02. 54(1):21–28.
Article6. Levy EI, Ecker RD, Horowitz MB, Gupta R, Hanel RA, Sauvageau E, et al. Stent-assisted intracranial recanalization for acute stroke: early results. Neurosurgery. 2006. 03. 58(3):458–463.
Article7. Menon BK, Kochar P, Ah-Seng A, Almekhlafi MA, Modi J, Wong JH, et al. Initial experience with a self-expanding retrievable stent for recanalization of large vessel occlusions in acute ischemic stroke. Neuroradiology. 2012. 02. 54(2):147–154.
Article8. Park H, Hwang GJ, Jin SC, Jung CK, Bang JS, Han MK, et al. A retrieval thrombectomy technique with the Solitaire stent in a large cerebral artery occlusion. Acta Neurochir (Wien). 2011. 08. 153(8):1625–1631.
Article9. Penumbra Pivotal Stroke Trial Investigators. The penumbra pivotal stroke trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke. 2009. 08. 40(8):2761–2768.10. Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke. 2007. 03. 38(3):967–973.11. Roth C, Papanagiotou P, Behnke S, Walter S, Haass A, Becker C, et al. Stent-assisted mechanical recanalization for treatment of acute intracerebral artery occlusions. Stroke. 2010. 11. 41(11):2559–2567.
Article12. Smith WS, Sung G, Saver J, Budzik R, Duckwiler G, Liebeskind DS, et al. Mechanical Thrombectomy for Acute Ischemic Stroke: Final Results of the Multi MERCI Trial. Stroke. 2008. 04. 39(4):1205–1212.13. Tomsick T, Broderick J, Carrozella J, Khatri P, Hill M, Palesch Y, et al. Revascularization results in the interventional management of stroke II trial. AJNR Am J Neuroradiol. 2008. 03. 29(3):582–587.
Article14. Zaidat OO, Suarez JI, Sunshine JL, Tarr RW, Alexander MJ, Smith TP, et al. Thrombolytic therapy of acute ischemic stroke: correlation of angiographic recanalization with clinical outcome. AJNR Am J Neuroradiol. 2005. 04. 26(4):880–884.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Limitations of Thrombectomy with Solitaire(TM) AB as First-line Treatment in Acute Ischemic Stroke: A Single Center Experience
- Safety and Efficacy of Mechanical Thrombectomy with Solitaire Stent Retrieval for Acute Ischemic Stroke: A Systematic Review
- Mechanical Thrombectomy Using a Solitaire Stent in Acute Ischemic Stroke: The Relationship between the Visible Antegrade Flow on First Device Deployment and Final Success in Revascularization
- Adjuvant Tirofiban Injection Through Deployed Solitaire Stent As a Rescue Technique After failed Mechanical Thrombectomy in Acute Stroke
- Refinement of a Thrombectomy Technique to Treat Acute Ischemic Stroke: Technical Note on Microcatheter Advance during Retrieving Self-Expandable Stent