Ann Surg Treat Res.
2015 Feb;88(2):86-91. 10.4174/astr.2015.88.2.86.
Can intravenous patient-controlled analgesia be omitted in patients undergoing laparoscopic surgery for colorectal cancer?
- Affiliations
-
- 1Colorectal Cancer Center, Kyungpook National University Hospital, Kyungpook National University School of Medicine, Daegu, Korea. kyuschoi@mail.knu.ac.kr
- 2Department of Anesthesia and Pain Medicine, Kyungpook National University Hospital, Kyungpook National University School of Medicine, Daegu, Korea.
- KMID: 1804125
- DOI: http://doi.org/10.4174/astr.2015.88.2.86
Abstract
- PURPOSE
Opioid-based intravenous patient-controlled analgesia (IV-PCA) is a popular method of postoperative analgesia, but many patients suffer from PCA-related complications. We hypothesized that PCA was not essential in patients undergoing major abdominal surgery by minimal invasive approach.
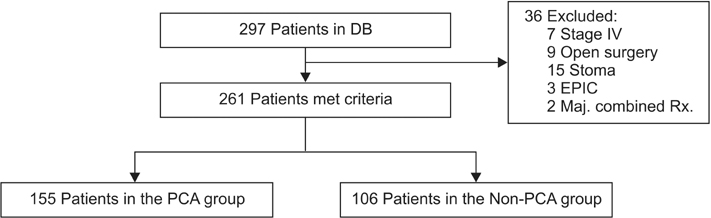
METHODS
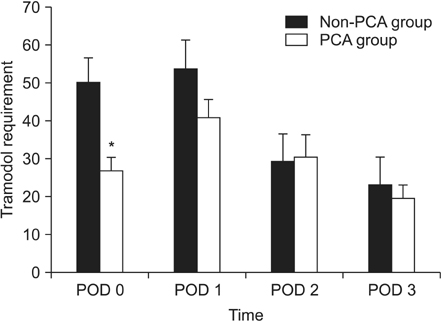
Between February 2013 and August 2013, 297 patients undergoing laparoscopic surgery for colorectal cancer were included in this retrospective comparative study. The PCA group received conventional opioid-based PCA postoperatively, and the non-PCA group received intravenous anti-inflammatory drugs (Tramadol) as necessary. Patients reported their postoperative pain using a subjective visual analogue scale (VAS). The PCA-related adverse effects and frequency of rescue analgesia were evaluated, and the recovery rates were measured.
RESULTS
Patients in the PCA group experienced less postoperative pain on days 4 and 5 after surgery than those in the non-PCA group (mean [SD] VAS: day 4, 6.2 [0.3] vs. 7.0 [0.3], P = 0.010; and day 5, 5.1 [0.2] vs. 5.5 [0.2], P = 0.030, respectively). Fewer patients in the non-PCA group required additional parenteral analgesia (41 of 93 patients vs. 53 of 75 patients, respectively), and none in the non-PCA group required rescue PCA postoperatively. The incidence of postoperative nausea and vomiting was significantly higher in the non-PCA group than in the PCA group (P < 0.001). The mean (range) length of hospital stay was shorter in the non-PCA group (7.9 [6-10] days vs. 8.7 [7-16] days, respectively, P = 0.03).
CONCLUSION
Our Results suggest that IV-PCA may not be necessary in selected patients those who underwent minimal invasive surgery for colorectal cancer.
MeSH Terms
Figure
Reference
-
1. Crisp CC, Bandi S, Kleeman SD, Oakley SH, Vaccaro CM, Estanol MV, et al. Patient-controlled versus scheduled, nurse-administered analgesia following vaginal reconstructive surgery: a randomized trial. Am J Obstet Gynecol. 2012; 207:433.e1–433.e6.2. Kim SH, Shin YS, Oh YJ, Lee JR, Chung SC, Choi YS. Risk assessment of postoperative nausea and vomiting in the intravenous patient-controlled analgesia environment: predictive values of the Apfel's simplified risk score for identification of high-risk patients. Yonsei Med J. 2013; 54:1273–1281.3. Grass JA. Patient-controlled analgesia. Anesth Analg. 2005; 101(5):Suppl. S44–S61.4. Fero KE, Jalota L, Hornuss C, Apfel CC. Pharmacologic management of postoperative nausea and vomiting. Expert Opin Pharmacother. 2011; 12:2283–2296.5. Kim JH, Jang SY, Kim MJ, Lee SY, Yoon JS. Comparison of pain-relieving effects of fentanyl versus ketorolac after eye amputation surgery. Korean J Ophthalmol. 2013; 27:229–234.6. Rosen M. The genesis, development and current usage of patient-controlled analgesia (PCA). Anaesth News. 2009; 267:9–11.7. Kum CK, Wong CW, Goh PM, Ti TK. Comparative study of pain level and analgesic requirement after laparoscopic and open cholecystectomy. Surg Laparosc Endosc. 1994; 4:139–141.8. Abraham NS, Young JM, Solomon MJ. Meta-analysis of short-term outcomes after laparoscopic resection for colorectal cancer. Br J Surg. 2004; 91:1111–1124.9. Veldkamp R, Gholghesaei M, Bonjer HJ, Meijer DW, Buunen M, Jeekel J, et al. Laparoscopic resection of colon Cancer: consensus of the European Association of Endoscopic Surgery (EAES). Surg Endosc. 2004; 18:1163–1185.10. Kim WR, Baek SJ, Kim CW, Jang HA, Cho MS, Bae SU, et al. Comparative study of oncologic outcomes for laparoscopic vs. open surgery in transverse colon cancer. Ann Surg Treat Res. 2014; 86:28–34.11. Johns N, O'Neill S, Ventham NT, Barron F, Brady RR, Daniel T. Clinical effectiveness of transversus abdominis plane (TAP) block in abdominal surgery: a systematic review and meta-analysis. Colorectal Dis. 2012; 14:e635–e642.12. Tilleul P, Aissou M, Bocquet F, Thiriat N, le Grelle O, Burke MJ, et al. Cost-effectiveness analysis comparing epidural, patient-controlled intravenous morphine, and continuous wound infiltration for postoperative pain management after open abdominal surgery. Br J Anaesth. 2012; 108:998–1005.13. Palmer P, Ji X, Stephens J. Cost of opioid intravenous patient-controlled analgesia: results from a hospital database analysis and literature assessment. Clinicoecon Outcomes Res. 2014; 6:311–318.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Nei-Guan acupressure on Nausea and Vomiting in Patients undergoing laparoscopic prostatectomy with Intravenous Patient Controlled Analgesia
- Comparison of Ramosetron Dose in Patients with Postoperative Nausea and Vomiting Who Received Oxycodone-Based Intravenous Patient-Controlled Analgesia after Undergoing Gynecological Laparoscopic Surgery
- Comparison of oxycodone and fentanyl for postoperative patient-controlled analgesia after laparoscopic gynecological surgery
- Efficacy and Safety of Ramosetron Injection for Nausea and Vomiting in Colorectal-Cancer Patients Undergoing a Laparoscopic Colectomy: A Randomized, Double-Blind, Comparative Study
- Comparison of Postoperative Analgesia and Side Effects by Patient-Controlled Epidural and Intravenous Analgesia after Cesarean Section