Korean J Hepatobiliary Pancreat Surg.
2015 Feb;19(1):25-29. 10.14701/kjhbps.2015.19.1.25.
Pneumatosis intestinalis after adult living donor liver transplantation: report of three cases and collective literature review
- Affiliations
-
- 1Department of Surgery, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- 2Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- KMID: 1802236
- DOI: http://doi.org/10.14701/kjhbps.2015.19.1.25
Abstract
- BACKGROUNDS/AIMS
Pneumatosis intestinalis (PI) is a condition in which multiple gas-filled mural cysts develop in the gastrointestinal tract. Although its exact etiology remains obscure, PI is rarely observed in liver transplant (LT) recipients.
METHODS
In 317 cases of adult living donor LT (LDLT) performed during 2011, PI developed in three patients during the 3 year follow-up.
RESULTS
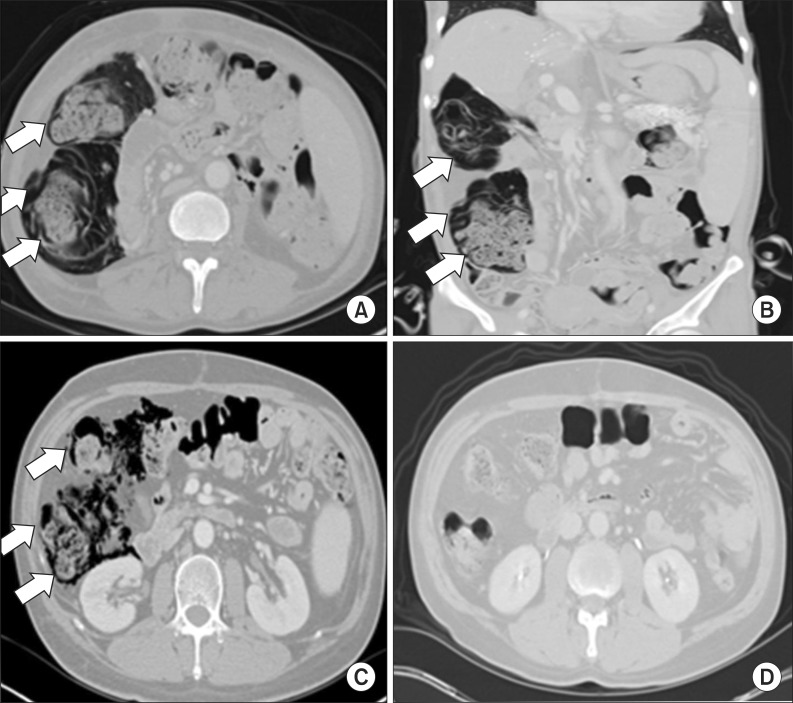
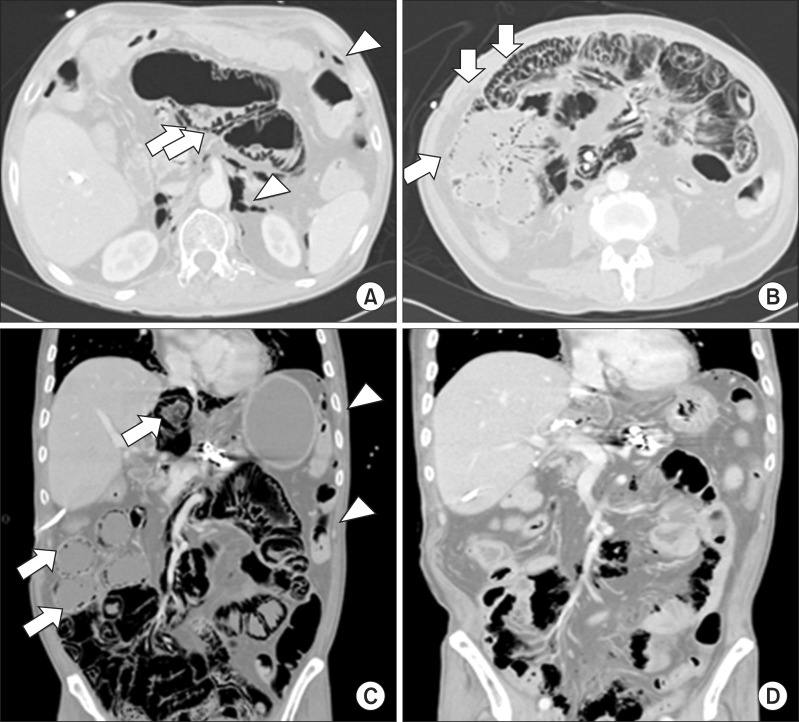
Of these three patients, the two who demonstrated PI at 6 weeks and 2 months after LT, respectively, were asymptomatic and showed no signs of secondary complications. Diagnosis was made incidentally using abdominal radiographs and computed tomography (CT) scans. PI was identified in the right ascending colon with concomitant pneumoperitoneum. These two patients received supportive care and maintained a regular diet. Follow-up CT scans demonstrated spontaneous resolution of PI with no complications. The third patient was admitted to the emergency room 30 months after LDLT. His symptoms included poor oral intake and intermittent abdominal pain with no passage of gas. Abdominal radiography and CT scans demonstrated PI in the entire small bowel, with small bowel dilatation, pneumoperitoneum, and pneumoretroperitoneum, but no peritonitis. Physical examination revealed abdominal distension but no tenderness or rebound tenderness. After 1 week of conservative treatment, including bowel rest and antibiotics therapy, PI and pneumoperitoneum resolved spontaneously without complications.
CONCLUSIONS
We suggest that adult LDLT recipients who develop asymptomatic or symptomatic PI with no signs of secondary complications can be successfully managed with conservative treatment.
MeSH Terms
-
Abdominal Pain
Adult*
Anti-Bacterial Agents
Colon, Ascending
Diagnosis
Diet
Dilatation
Emergency Service, Hospital
Follow-Up Studies
Gastrointestinal Tract
Humans
Liver
Liver Transplantation*
Living Donors*
Peritonitis
Physical Examination
Pneumoperitoneum
Radiography, Abdominal
Retropneumoperitoneum
Tomography, X-Ray Computed
Anti-Bacterial Agents
Figure
Reference
-
1. Ecker JA, Williams RG, Clay KL. Pneumatosis cystoides intestinalis--bullous emphysema of the intestine. A review of the literature. Am J Gastroenterol. 1971; 56:125–136. PMID: 4938483.2. Koss LG. Abdominal gas cysts (pneumatosis cystoides intestinorum hominis); an analysis with a report of a case and a critical review of the literature. AMA Arch Pathol. 1952; 53:523–549. PMID: 14923068.3. Galm O, Fabry U, Adam G, Osieka R. Pneumatosis intestinalis following cytotoxic or immunosuppressive treatment. Digestion. 2001; 64:128–132. PMID: 11684828.
Article4. Andorsky RI. Pneumatosis cystoides intestinalis after organ transplantation. Am J Gastroenterol. 1990; 85:189–194. PMID: 2405645.5. Sachse RE, Burke GW 3rd, Jonas M, Milgrom M, Miller J. Benign pneumatosis intestinalis with subcutaneous emphysema in a liver transplant recipient. Am J Gastroenterol. 1990; 85:876–879. PMID: 2371990.6. Janssen DA, Kalayoglu M, Sollinger HW. Pneumatosis cystoides intestinalis following lactulose and steroid treatment in a liver transplant patient with an intermittently enlarged scrotum. Transplant Proc. 1987; 19:2949–2952. PMID: 3551239.7. Wiesner W, Mortelé KJ, Glickman JN, Ji H, Ros PR. Pneumatosis intestinalis and portomesenteric venous gas in intestinal ischemia: correlation of CT findings with severity of ischemia and clinical outcome. AJR Am J Roentgenol. 2001; 177:1319–1323. PMID: 11717075.8. Kwon HJ, Kim KW, Song GW, Kim DY, Chung SY, Hwang S, et al. Pneumatosis intestinalis after liver transplantation. Eur J Radiol. 2011; 80:629–636. PMID: 20807675.
Article9. Jamart J. Pneumatosis cystoides intestinalis. A statistical study of 919 cases. Acta Hepatogastroenterol (Stuttg). 1979; 26:419–422. PMID: 525221.10. Hepgur M, Ahluwalia MS, Anne N, Thomas J, Liu H, Schiff MD, et al. Medical management of pneumatosis intestinalis in patients undergoing allogeneic blood and marrow transplantation. Bone Marrow Transplant. 2011; 46:876–879. PMID: 20871638.
Article11. Jones B, Fishman EK, Kramer SS, Siegelman SS, Saral R, Beschorner WE, et al. Computed tomography of gastrointestinal inflammation after bone marrow transplantation. AJR Am J Roentgenol. 1986; 146:691–695. PMID: 3513488.
Article12. Knechtle SJ, Davidoff AM, Rice RP. Pneumatosis intestinalis. Surgical management and clinical outcome. Ann Surg. 1990; 212:160–165. PMID: 2375647.13. Koep LJ, Peters TG, Starzl TE. Major colonic complications of hepatic transplantation. Dis Colon Rectum. 1979; 22:218–220. PMID: 380946.
Article14. King S, Shuckett B. Sonographic diagnosis of portal venous gas in two pediatric liver transplant patients with benign pneumatosis intestinalis. Case reports and literature review. Pediatr Radiol. 1992; 22:577–578. PMID: 1491932.15. Kim JM, Park Y, Joh JW, Kwon CH, Kim SJ, Hong SH, et al. Pneumatosis intestinalis after adult liver transplantation. J Korean Surg Soc. 2011; 80(Suppl 1):S47–S50. PMID: 22066083.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pneumatosis Cystoides Intestinalis after Liver Transplantation
- A Case of Primary Pneumatosis Cystoides Intestinalis in a Patient with Chronic Abdominal Pain
- Pneumatosis intestinalis after adult liver transplantation
- Left at right heterotopic implantation of left liver graft in adult-to-adult living donor liver transplantation: the technical concern for decision-making
- Liver retransplantation for adult recipients