J Korean Surg Soc.
2011 Jun;80(Suppl 1):S47-S50. 10.4174/jkss.2011.80.Suppl1.S47.
Pneumatosis intestinalis after adult liver transplantation
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jw.joh@samsung.com
- 2Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Organ Transplant Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2096650
- DOI: http://doi.org/10.4174/jkss.2011.80.Suppl1.S47
Abstract
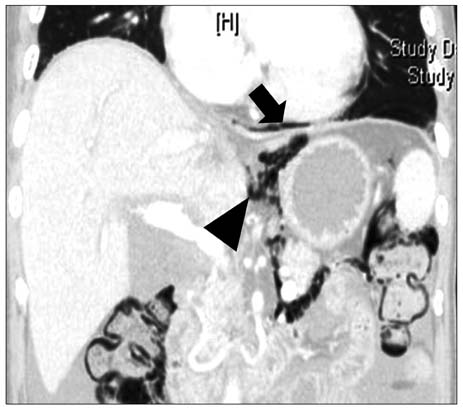
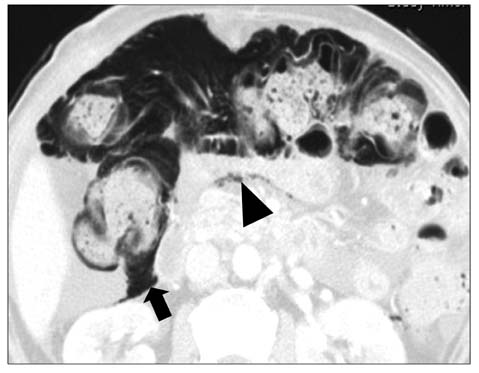
- Pneumatosis intestinalis is an uncommon disorder characterized by an accumulation of gas in the bowel wall. We described three cases undertaking liver transplantation. The patients developed diarrhea in three cases and high fever in two. An abdominal X-ray and computed tomography scan demonstrated extensive pneumatosis intestinalis in the colon with pneumoperitoneum mimicking hollow organ perforation. However, the patients had no abdominal symptoms and there was no evidence of peritonitis. The infection work-up was negative except one case with cytomegalovirus antigenemia. After one week of conservative management including bowel rest and antibiotic therapy, their pneumoperitoneum resolved spontaneously without any complication. Pneumatosis intestinalis should be considered as a differential diagnosis after adult liver transplantation with patients suffering from watery diarrhea and fever. Pneumoperitoneum, air-density in mesentery and retroperitoneum in patients with pneumatosis intestinalis without signs of peritonitis improved with conservative management, which included bowel rest and antibiotic therapy.
MeSH Terms
Figure
Cited by 1 articles
-
Pneumatosis intestinalis after adult living donor liver transplantation: report of three cases and collective literature review
Cheon-Soo Park, Shin Hwang, Dong-Hwan Jung, Gi-Won Song, Deok-Bog Moon, Chul-Soo Ahn, Gil-Chun Park, Ki-Hun Kim, Tae-Yong Ha, Sung-Gyu Lee
Korean J Hepatobiliary Pancreat Surg. 2015;19(1):25-29. doi: 10.14701/kjhbps.2015.19.1.25.
Reference
-
1. Burress GC, Ben-Ami T, Whitington PF. Pneumatosis intestinalis in infants after orthotopic liver transplantation. J Pediatr Gastroenterol Nutr. 1996. 23:577–582.2. Janssen DA, Kalayoglu M, Sollinger HW. Pneumatosis cystoides intestinalis following lactulose and steroid treatment in a liver transplant patient with an intermittently enlarged scrotum. Transplant Proc. 1987. 19:2949–2952.3. King S, Shuckett B. Sonographic diagnosis of portal venous gas in two pediatric liver transplant patients with benign pneumatosis intestinalis: case reports and literature review. Pediatr Radiol. 1992. 22:577–578.4. Sachse RE, Burke GW 3rd, Jonas M, Milgrom M, Miller J. Benign pneumatosis intestinalis with subcutaneous emphysema in a liver transplant recipient. Am J Gastroenterol. 1990. 85:876–879.5. Koep LJ, Peters TG, Starzl TE. Major colonic complications of hepatic transplantation. Dis Colon Rectum. 1979. 22:218–220.6. Andorsky RI. Pneumatosis cystoides intestinalis after organ transplantation. Am J Gastroenterol. 1990. 85:189–194.7. Jamart J. Pneumatosis cystoides intestinalis: a statistical study of 919 cases. Acta Hepatogastroenterol (Stuttg). 1979. 26:419–422.8. Greenstein AJ, Nguyen SQ, Berlin A, Corona J, Lee J, Wong E, et al. Pneumatosis intestinalis in adults: management, surgical indications, and risk factors for mortality. J Gastrointest Surg. 2007. 11:1268–1274.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pneumatosis Cystoides Intestinalis after Liver Transplantation
- A Case of Primary Pneumatosis Cystoides Intestinalis in a Patient with Chronic Abdominal Pain
- A Case of Pneumatosis Cystoides Intestinalis in a Patient with Systemic Lupus Erythematosus
- Asymptomatic Pneumatosis Intestinalis in Immune-competent Adult
- A Case of Nonspecific Interstitial Pneumonia Complicated with Spontaneous Pneumomediastinum, Subcutaneous Emphysema and Pneumatosis Interstinalis