Korean J Hepatobiliary Pancreat Surg.
2014 Nov;18(4):152-158. 10.14701/kjhbps.2014.18.4.152.
Surgical outcomes of multifocal branch duct intraductal papillary mucinous neoplasms of pancreas
- Affiliations
-
- 1Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. drksc@amc.seoul.kr
- KMID: 1802231
- DOI: http://doi.org/10.14701/kjhbps.2014.18.4.152
Abstract
- BACKGROUNDS/AIMS
Appropriate management for multifocal branch duct type intraductal papillary mucinous neoplasms (BD-IPMNs) of the pancreas is still controversial. This study was intended to reveal surgical outcomes of surgical resection for multifocal BD-IPMNs, with BD-IPMNs in the remnant pancreas.
METHODS
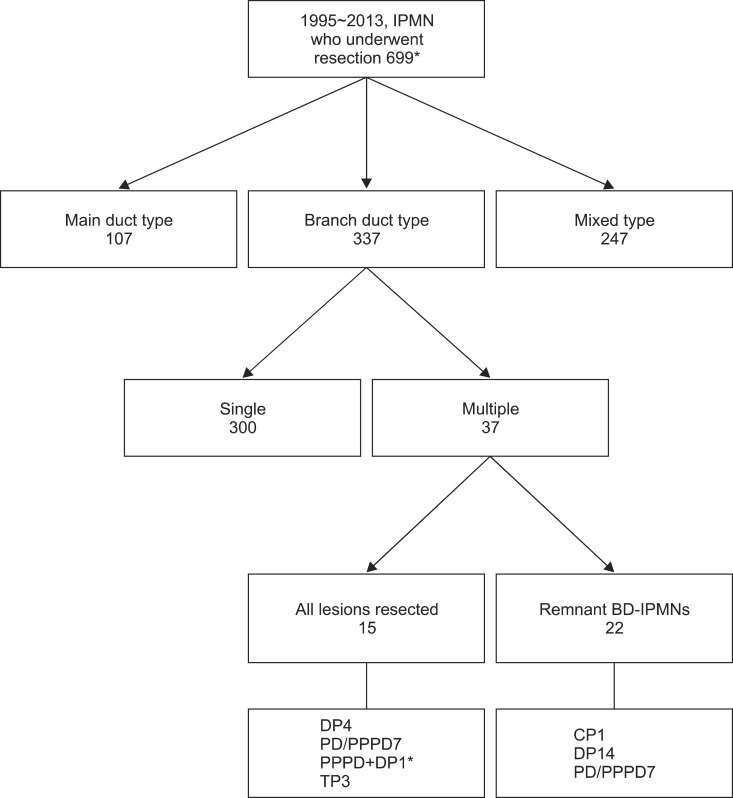
Between January 1995 and December 2013, 699 patients underwent the pancreatic resection due to IPMN of pancreas in our institution. Among them, 37 patients showed multifocal BD-IPMNs. After excluding patients who had BD-IPMNs completely resected, medical records of 22 patients with remained BD-IPMNs in the remnant pancreas were retrospectively reviewed.
RESULTS
Mean patient age was 65+/-6.4 years. Types of surgery included central pancreatectomy (n=1), distal pancreatectomy (n=14), and standard pylorus-preserving pancreaticoduodenectomy (n=7). Specimen pathology showed that IPMN was either at low/intermediate-grade dysplasia (n=17) or at high-grade dysplasia (n=2). Three patients had IPMN associated with invasive carcinoma. Their mean follow-up period was 40.4 months. During follow-up, one mortality occurred 35.2 months after the operation which was not associated with IPMN. There was no clinically significant disease progression or recurrence of IPMN in the remnant pancreas during the follow-up period.
CONCLUSIONS
Our results support that we can safely preserve the pancreas parenchyma with multifocal BD-IPMNs. Benign-looking multifocal BD-IPMNs in the remnant pancreas do not affect the survival of patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012; 12:183–197. PMID: 22687371.
Article2. Goh BK, Tan DM, Ho MM, Lim TK, Chung AY, Ooi LL. Utility of the sendai consensus guidelines for branch-duct intraductal papillary mucinous neoplasms: a systematic review. J Gastrointest Surg. 2014; 18:1350–1357. PMID: 24668367.
Article3. Jang JY, Park T, Lee S, Kang MJ, Lee SY, Lee KB, et al. Validation of international consensus guidelines for the resection of branch duct-type intraductal papillary mucinous neoplasms. Br J Surg. 2014; 101:686–692. PMID: 24668442.
Article4. Aso T, Ohtsuka T, Matsunaga T, Kimura H, Watanabe Y, Tamura K, et al. "High-risk stigmata" of the 2012 international consensus guidelines correlate with the malignant grade of branch duct intraductal papillary mucinous neoplasms of the pancreas. Pancreas. 2014; 43:1239–1243. PMID: 25036910.
Article5. Schmidt CM, White PB, Waters JA, Yiannoutsos CT, Cummings OW, Baker M, et al. Intraductal papillary mucinous neoplasms: predictors of malignant and invasive pathology. Ann Surg. 2007; 246:644–651. PMID: 17893501.6. Rodriguez JR, Salvia R, Crippa S, Warshaw AL, Bassi C, Falconi M, et al. Branch-duct intraductal papillary mucinous neoplasms: observations in 145 patients who underwent resection. Gastroenterology. 2007; 133:72–79. PMID: 17631133.
Article7. Bosmanm FT, Carneiro F, Hruban RH, Theise ND. WHO classification of tumours of the digestive system. 4th ed. Lyon, France: IARC Press;2010.8. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, et al. AJCC cancer staging manual. 7th ed. New York: Springer-Verlag;2010.9. Maguchi H, Tanno S, Mizuno N, Hanada K, Kobayashi G, Hatori T, et al. Natural history of branch duct intraductal papillary mucinous neoplasms of the pancreas: a multicenter study in Japan. Pancreas. 2011; 40:364–370. PMID: 21289527.10. Kobayashi G, Fujita N, Maguchi H, Tanno S, Mizuno N, Hanada K, et al. Natural history of branch duct intraductal papillary mucinous neoplasm with mural nodules: a Japan pancreas society multicenter study. Pancreas. 2014; 43:532–538. PMID: 24717801.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraductal Papillary Mucinous Tumor Simultaneously Involving the Liver and Pancreas: A Case Report
- Photodynamic Therapy Followed by Left Hepatectomy Used to Treat an Intraductal Papillary Mucinous Neoplasm of the Bile Duct
- An Intraductal Papillary Mucinous Tumors (IPMT) of the Pancreas: Clinical, Radiologie, and Pathologie Findings Acccrding to Its Subtypes
- Surgical Management of Intraductal Papillary Mucinous Neoplasms
- Comparison of Mucinous Cystic Tumor and Intraductal Papillary Mucinous Tumor