Yonsei Med J.
2013 Nov;54(6):1516-1523. 10.3349/ymj.2013.54.6.1516.
Autologous Platelet-Poor Plasma Gel for Injection Laryngoplasty
- Affiliations
-
- 1Department of Otolaryngology, Gyeongsang National University, Jinju, Korea.
- 2Institute of Health Sciences, Gyeongsang National University, Jinju, Korea.
- 3Department of Otorhinolaryngology-Head & Neck Surgery, College of Medicine, Dankook University, Cheonan, Korea.
- 4Department of Otorhinolaryngology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. entlsh@hanmail.net
- 5Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. hansin.jeong@gmail.com
- KMID: 1798152
- DOI: http://doi.org/10.3349/ymj.2013.54.6.1516
Abstract
- PURPOSE
To overcome the potential disadvantages of the use of foreign materials and autologous fat or collagen, we introduce here an autologous plasma gel for injection laryngoplasty. The purpose of this study was to present a new injection material, a plasma gel, and to discuss its clinical effectiveness.
MATERIALS AND METHODS
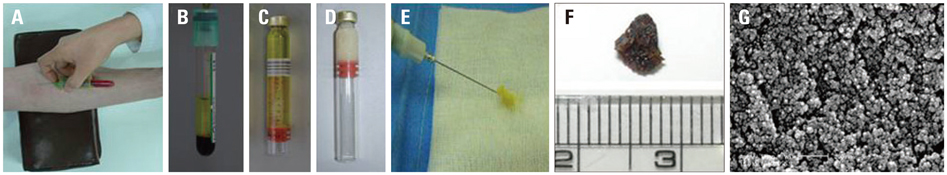
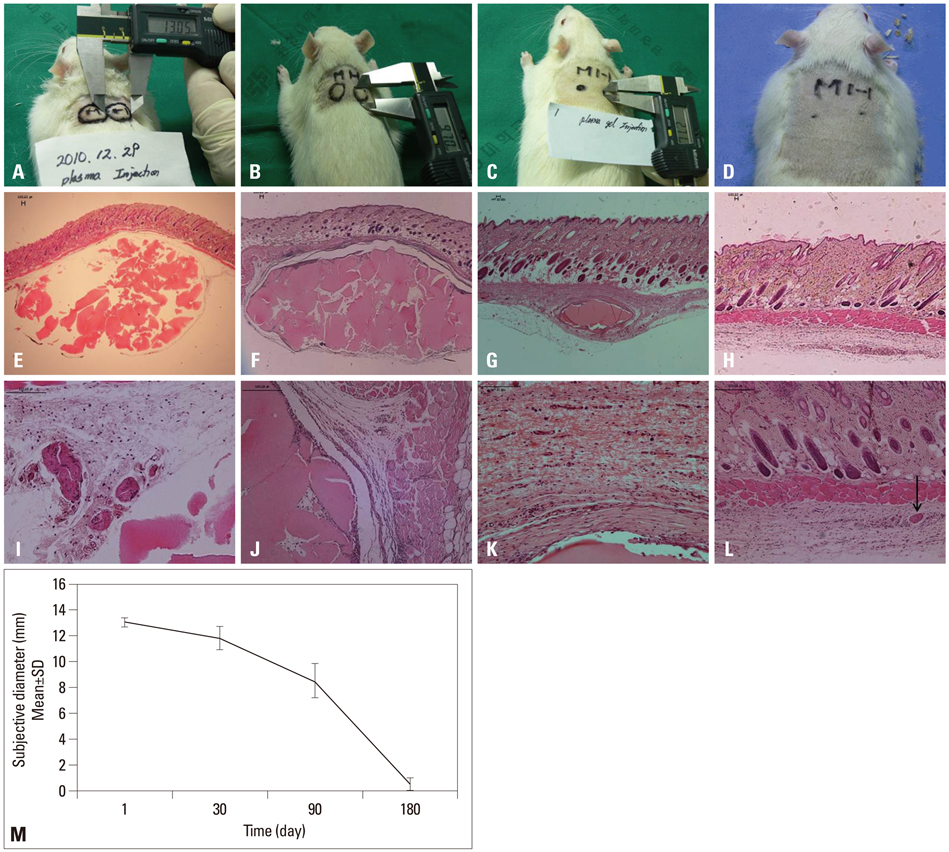
From 2 mL of blood, the platelet poor serum layer was collected and heated at 100degrees C for 12 min to form a plasma gel. The plasma gel was then injected into a targeted site; the safety and efficacy thereof were evaluated in 30 rats. We also conducted a phase I/II clinical study of plasma gel injection laryngoplasty in 11 unilateral vocal fold paralysis patients.
RESULTS
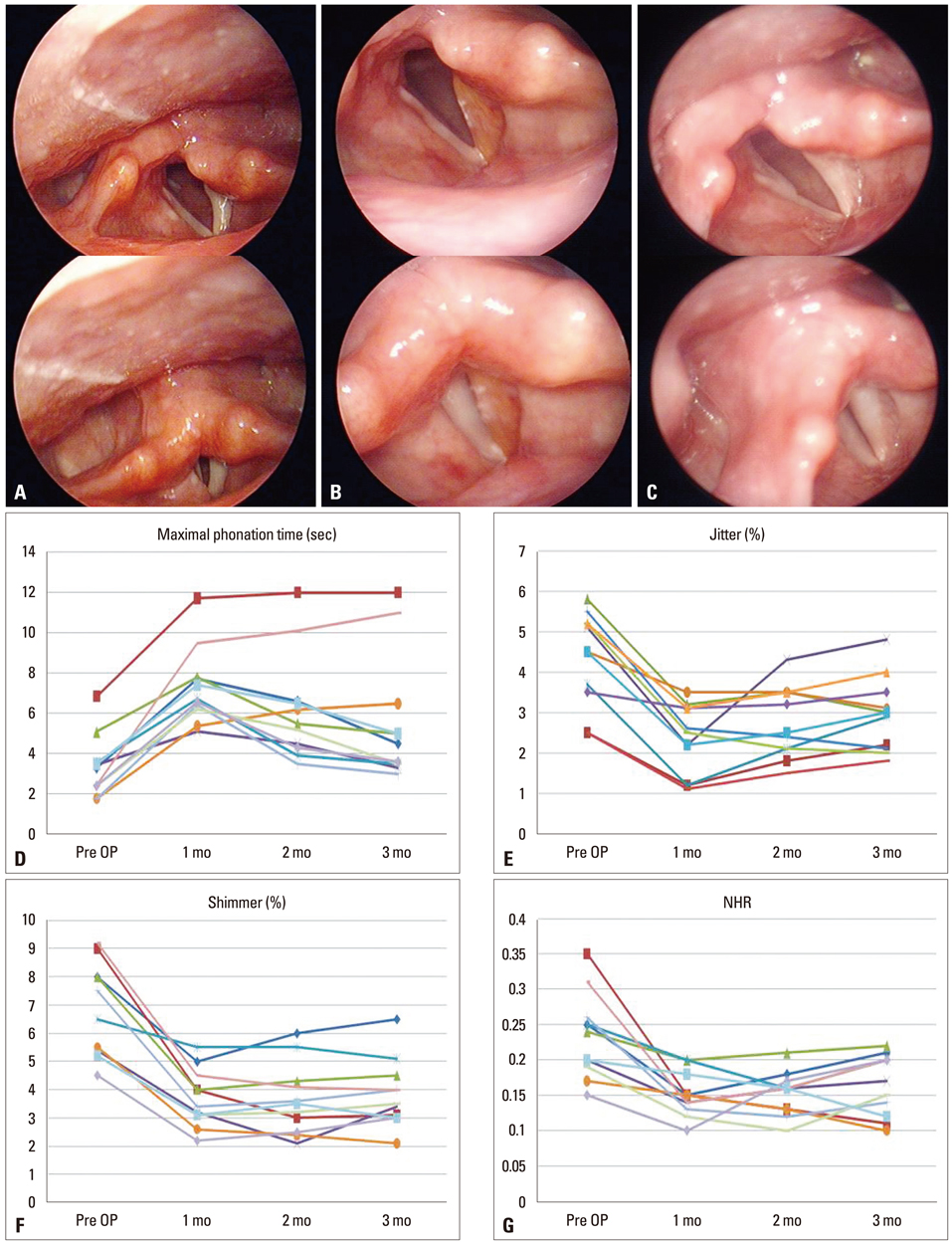
The plasma gel was semi-solid and an easily injectable material. Of note, plasma gel maintains the same consistency for up to 1 year in a sealed bottle. However, exposure to room air causes the plasma gel to disappear within 1 month. In our animal study, the autologous plasma gel remained in situ for 6 months in animals with minimal inflammation. Clinical study showed that vocal cord palsy was well compensated for with the plasma gel in all patients at two months after injection with no significant complications. Jitter, shimmer, maximum, maximum phonation time (MPT) and mean voice handicap index (VHI) also improved significantly after plasma gel injection. However, because the injected plasma gel was gradually absorbed, 6 patients needed another injection, while the gel remained in place in 2 patients.
CONCLUSION
Injection laryngoplasty with autologous plasma gel may be a useful and safe treatment option for temporary vocal cord palsy.
MeSH Terms
Figure
Cited by 1 articles
-
Calcium Hydroxylapatite Pulmonary Embolism after Percutaneous Injection Laryngoplasty
Seong Jun Won, Seung Hoon Woo
Yonsei Med J. 2017;58(6):1245-1248. doi: 10.3349/ymj.2017.58.6.1245.
Reference
-
1. Brunnings W. Uber eine neue Behandlungsmethode der Rekurrenslahmung. Verhandl Ver Dtsch Laryngol. 1911; 18:93–151.2. Lewy RB. Tracheotomy avoidance. Glycerine vocal cord injection. Arch Otolaryngol. 1970; 92:502–504.
Article3. Kwon TK, Rosen CA, Gartner-Schmidt J. Preliminary results of a new temporary vocal fold injection material. J Voice. 2005; 19:668–673.
Article4. Mallur PS, Rosen CA. Vocal fold injection: review of indications, techniques, and materials for augmentation. Clin Exp Otorhinolaryngol. 2010; 3:177–182.
Article5. Sulica L, Rosen CA, Postma GN, Simpson B, Amin M, Courey M, et al. Current practice in injection augmentation of the vocal folds: indications, treatment principles, techniques, and complications. Laryngoscope. 2010; 120:319–325.
Article6. Hill DP, Meyers AD, Harris J. Autologous fat injection for vocal cord medialization in the canine larynx. Laryngoscope. 1991; 101(4 Pt 1):344–348.
Article7. Ford CN, Staskowski PA, Bless DM. Autologous collagen vocal fold injection: a preliminary clinical study. Laryngoscope. 1995; 105(9 Pt 1):944–948.
Article8. Rihkanen H. Vocal fold augmentation by injection of autologous fascia. Laryngoscope. 1998; 108(1 Pt 1):51–54.
Article9. Lee BJ, Wang SG, Goh EK, Chon KM, Lee CH. Intracordal injection of autologous auricular cartilage in the paralyzed canine vocal fold. Otolaryngol Head Neck Surg. 2004; 131:34–43.
Article10. Shindo ML, Zaretsky LS, Rice DH. Autologous fat injection for unilateral vocal fold paralysis. Ann Otol Rhinol Laryngol. 1996; 105:602–606.
Article11. Lee SW, Kim JW, Koh YW, Shim SS, Son YI. Comparative Analysis of Efficiency of Injection Laryngoplasty Technique for with or without Neck Treatment Patients: A Transcartilaginous Approach Versus the Cricothyroid Approach. Clin Exp Otorhinolaryngol. 2010; 3:37–41.
Article12. Goodman GJ. Blood transfer: the use of autologous blood as a chromophore and tissue augmentation agent. Dermatol Surg. 2001; 27:857–862.
Article13. Margolis DJ, Kantor J, Santanna J, Strom BL, Berlin JA. Effectiveness of platelet releasate for the treatment of diabetic neuropathic foot ulcers. Diabetes Care. 2001; 24:483–488.
Article14. McAleer JP, Sharma S, Kaplan EM, Persich G. Use of autologous platelet concentrate in a nonhealing lower extremity wound. Adv Skin Wound Care. 2006; 19:354–363.
Article15. Zavadil DP, Satterlee CC, Costigan JM, Holt DW, Shostrom VK. Autologous platelet gel and platelet-poor plasma reduce pain with total shoulder arthroplasty. J Extra Corpor Technol. 2007; 39:177–182.16. Eppley BL, Pietrzak WS, Blanton M. Platelet-rich plasma: a review of biology and applications in plastic surgery. Plast Reconstr Surg. 2006; 118:147e–159e.
Article17. Pietrzak WS, Eppley BL. Platelet rich plasma: biology and new technology. J Craniofac Surg. 2005; 16:1043–1054.
Article18. Cillo JE Jr, Marx RE, Stevens MR. Evaluation of autologous platelet-poor plasma gel as a hemostatic adjunct after posterior iliac crest bone harvest. J Oral Maxillofac Surg. 2007; 65:1734–1738.
Article19. Floryan KM, Berghoff WJ. Intraoperative use of autologous platelet-rich and platelet-poor plasma for orthopedic surgery patients. AORN J. 2004; 80:668–674.
Article20. Man D, Plosker H, Winland-Brown JE. The use of autologous platelet-rich plasma (platelet gel) and autologous platelet-poor plasma (fibrin glue) in cosmetic surgery. Plast Reconstr Surg. 2001; 107:229–237.
Article21. Shim HS, Woo SH. Vocal fold hemorrhage in a CML patient after Glivec treatment. Acta Oncol. 2013; 52:866–868.
Article22. Luengo Gimeno F, Gatto S, Ferro J, Croxatto JO, Gallo JE. Preparation of platelet-rich plasma as a tissue adhesive for experimental transplantation in rabbits. Thromb J. 2006; 4:18.
Article23. Courey MS. Injection laryngoplasty. Otolaryngol Clin North Am. 2004; 37:121–138.
Article24. Homicz MR, Watson D. Review of injectable materials for soft tissue augmentation. Facial Plast Surg. 2004; 20:21–29.
Article25. Woo SH, Son YI, Lee SH, Park JJ, Kim JP. Comparative analysis on the efficiency of the injection laryngoplasty technique using calcium hydroxyapatite (CaHA): the thyrohyoid approach versus the cricothyroid approach. J Voice. 2013; 27:236–241.
Article26. Kim JP, Cho SJ, Son HY, Park JJ, Woo SH. Analysis of clinical feature and management of laryngeal fracture: recent 22 case review. Yonsei Med J. 2012; 53:992–998.
Article27. Lee EJ, Yang YS, Kim JS, Hong KH. A "boxer glove" contoured laryngeal amyloidosis. Clin Exp Otorhinolaryngol. 2012; 5:240–242.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Recalcitrant Medial and Lateral Epicondylitis with Autologous Platelet Rich Plasma; Preliminary Report
- The Vocal Fold Augmentation with Liposuctioned Autologous Fat
- Review of Injection Laryngoplasty as Treatment of Voice Disorders
- Intralesional Injection of Autologous Platelet-Rich Plasma as an Effective Regeneration Therapy: A Case Report of Chronic Wagner Grade 2 Diabetic Foot Ulcer
- Effect of Platelet-rich Plasma on Burn Wounds according to Time of Application: An Experimental Study on Rats