J Korean Foot Ankle Soc.
2022 Dec;26(4):187-191. 10.14193/jkfas.2022.26.4.187.
Intralesional Injection of Autologous Platelet-Rich Plasma as an Effective Regeneration Therapy: A Case Report of Chronic Wagner Grade 2 Diabetic Foot Ulcer
- Affiliations
-
- 1GC iMED Gang-Nam Clinic, Seoul, Korea
- KMID: 2536715
- DOI: http://doi.org/10.14193/jkfas.2022.26.4.187
Abstract
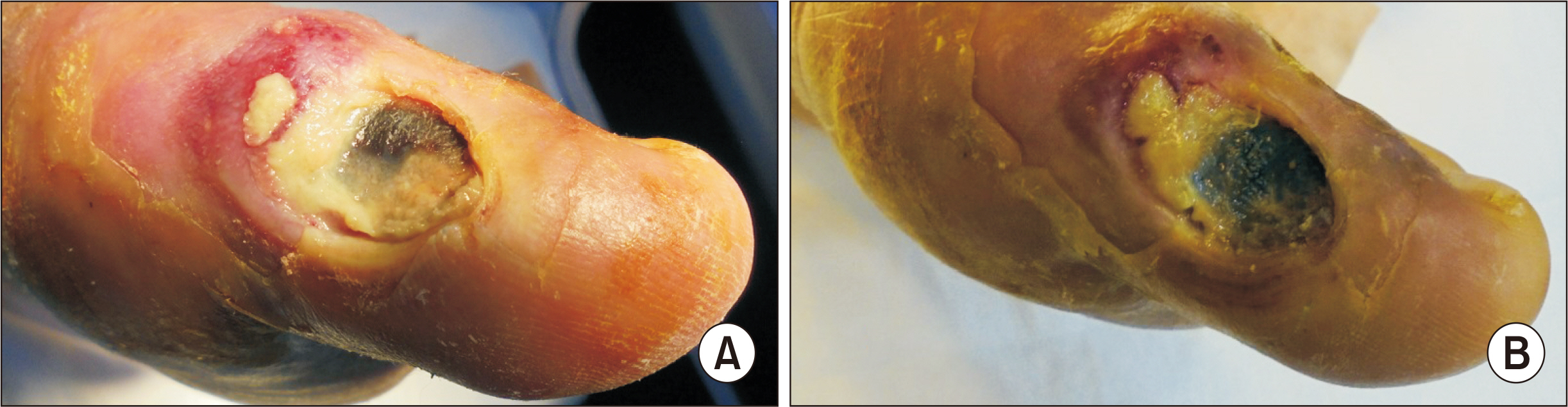
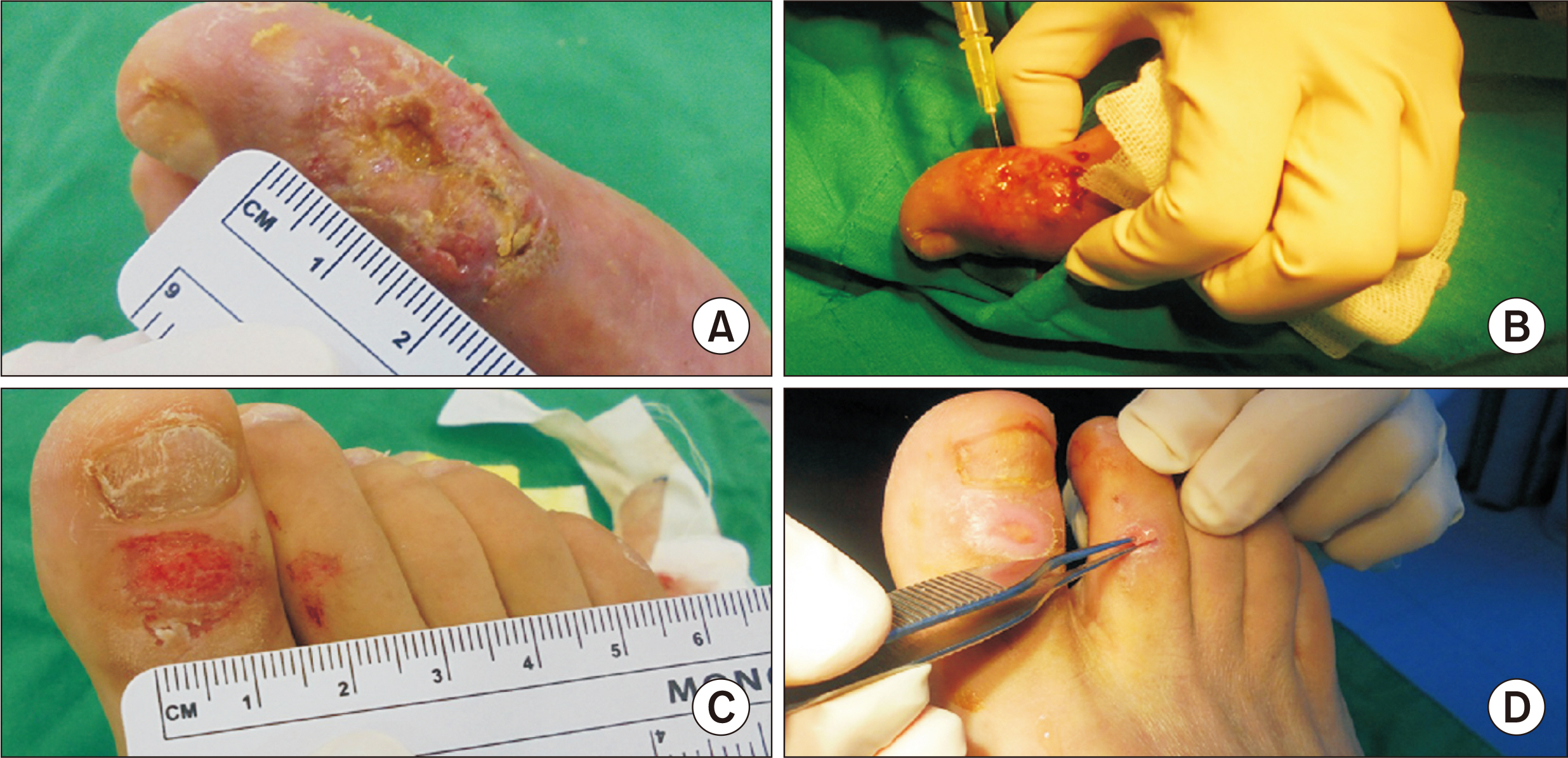
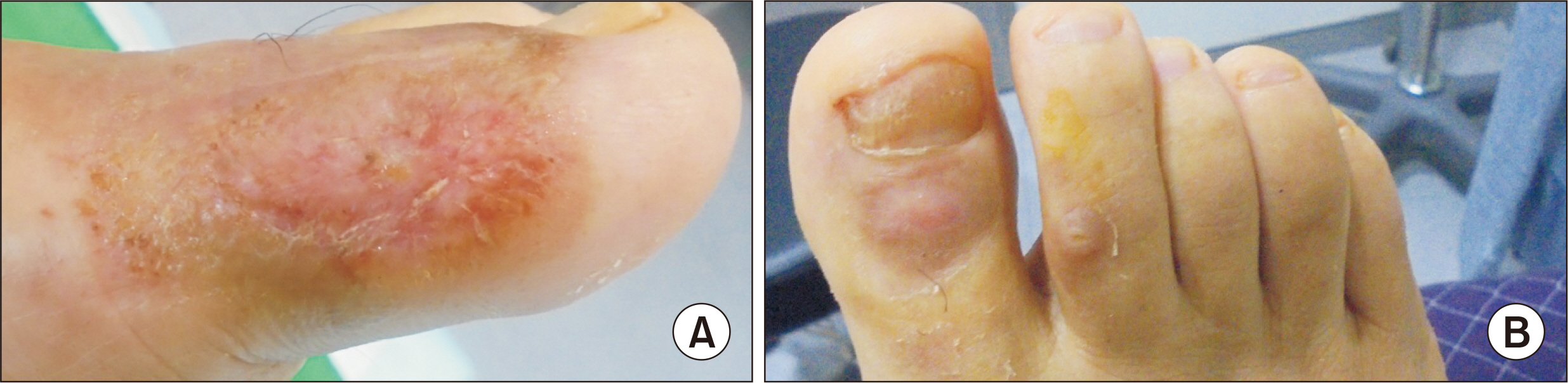
- The author experienced a case of autologous platelet-rich plasma (PRP) affecting the recovery of a chronic neuropathic diabetic foot ulcer combined with infection. A 65-year-aged male with uncontrolled diabetes presented with a Wagner grade 2 diabetic foot ulcer on his left forefoot of more than 2 weeks duration. Osteomyelitis, gangrene, and ischemia requiring acute intervention were absent. Although infection was controlled to a moderate degree, wound healing was unsatisfactory following surgical debridement and simple dressing. Therefore, intralesional autologous PRP injection was performed 5 times as an adjuvant regeneration therapy, and the recalcitrant ulcer healed in 3 months. Intralesional PRP injections are worthwhile as they promote wound regeneration, are evidence-based, safe, and can be easily performed in ambulatory care facilities.
Keyword
Figure
Reference
-
1. Andrews KL, Houdek MT, Kiemele LJ. 2015; Wound management of chronic diabetic foot ulcers: from the basics to regenerative medicine. Prosthet Orthot Int. 39:29–39. doi: 10.1177/0309364614534296. DOI: 10.1177/0309364614534296. PMID: 25614499.2. Milne TE, Schoen DE, Bower VM, Burrows SA, Westphal C, Gurr JM. 2013; Healing times of diabetic foot ulcers: investigating the influence of infection and peripheral arterial disease. J Diabet Foot Complicat. 5:29–38.3. Schaper NC, van Netten JJ, Apelqvist J, Bus SA, Hinchliffe RJ, Lipsky BA. 2020; Practical guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes Metab Res Rev. 36 Suppl 1:e3266. doi: 10.1002/dmrr.3266. DOI: 10.1002/dmrr.3266. PMCID: PMC7154668.4. Scimeca CL, Bharara M, Fisher TK, Kimbriel H, Armstrong DG. 2010; Novel use of platelet-rich plasma to augment curative diabetic foot surgery. J Diabetes Sci Technol. 4:1121–6. doi: 10.1177/193229681000400510. DOI: 10.1177/193229681000400510. PMID: 20920431. PMCID: PMC2956802.5. Everett E, Mathioudakis N. 2018; Update on management of diabetic foot ulcers. Ann N Y Acad Sci. 1411:153–65. doi: 10.1111/nyas.13569. DOI: 10.1111/nyas.13569. PMID: 29377202. PMCID: PMC5793889.6. Lipsky BA, Senneville É, Abbas ZG, Aragón-Sánchez J, Diggle M, Embil JM, et al. International Working Group on the Diabetic Foot (IWGDF). 2020; Guidelines on the diagnosis and treatment of foot infection in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 36 Suppl 1:e3280. doi: 10.1002/dmrr.3280. DOI: 10.1002/dmrr.3280. PMCID: PMC7154668.7. Kim MH, Byeon HS. 2019; Review for good platelet-rich plasma procedure in cosmetic dermatology and surgery. J Cosmet Med. 3:1–13. doi: 10.25056/JCM.2019.3.1.1. DOI: 10.25056/JCM.2019.3.1.1.8. Zimny S, Schatz H, Pfohl M. 2002; Determinants and estimation of healing times in diabetic foot ulcers. J Diabetes Complications. 16:327–32. doi: 10.1016/s1056-8727(01)00217-3. DOI: 10.1016/S1056-8727(01)00217-3. PMID: 12200075.9. Monami M, Ragghianti B, Nreu B, Lorenzoni V, Pozzan M, Silverii A, et al. Major amputation in non-healing ulcers: outcomes and economic issues. Data from a cohort of patients with diabetic foot ulcers. Int J Low Extrem Wounds. Published online April 28, 2022; doi: 10.1177/15347346221097283. DOI: 10.1177/15347346221097283. PMID: 35477285.10. Won SH, Min TH, Chun DI, Bae SY. The Academic Committee of Korean Foot and Ankle Society. 2022; Current trends in the treatment of diabetic foot: analysis of the Korean Foot and Ankle Society (KFAS) member survey. J Korean Foot Ankle Soc. 26:30–9. doi: 10.14193/jkfas.2022.26.1.30. DOI: 10.14193/jkfas.2022.26.1.30.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recalcitrant Cutaneous Ulcer of Comorbid Patient Treated with Platelet Rich Plasma: A Case Report
- A Case of Recalcitrant Ulcer Treated with Platelet-rich Plasma Therapy in a Patient with Phakomatosis Pigmentovascularis Type IIb
- Diabetic Foot Ulcer Recording Form Incorporating the Concepts of Wound Care and Treatment Plan
- Clinical Analysis of Chronic Ischemic Foot Ulcer using Ischemic Index with Flowmeter and Wagner Classification
- Hyaluronic Acid and Platelet-Rich Plasma Injections in Foot and Ankle Disorders