Dement Neurocogn Disord.
2013 Dec;12(4):94-99. 10.12779/dnd.2013.12.4.94.
The Association of Gait Disturbance and Cognitive Impairment
- Affiliations
-
- 1Korea University School of Medicine, Seoul, Korea.
- 2Department of Neurology, Korea University Anam Hospital, Seoul, Korea. kunu@korea.ac.kr
- KMID: 1797941
- DOI: http://doi.org/10.12779/dnd.2013.12.4.94
Abstract
- BACKGROUND
The incidence and prevalence of gait disturbance increases as age increases. The importance of cognitive aspects of gait disturbances has been studied in various types of dementia and MCI. This study was performed to identify relationship between cognitive impairment and change in gait, and investigate specific domains of cognitive function that may have affects in gait disturbance.
METHODS
Three hundred eighty three participants over 60 years old volunteered for the study. Three stages evaluation were performed, dementia screening and timed up and go test (TUG), work up for cognitive impairment and dementia, and classifying cognitive impairment and dementia into subcategories by evaluating cause of the disease. To evaluate cognitive impairment, MMSE-KC (MMSE in the Korean version of the CERAD assessment packet) and Korean version of Consortium to Establish a Registry of Alzheimer's Disease (CERAD-K) assessment were used. One hundred forty one people were excluded from study and 242 people were analyzed. Timed Up and Go test (TUG) was performed for evaluation of gait disturbance. Relationship in every subcategory of CERAD-K and TUG was studied by correlation and multiple logistic analysis.
RESULTS
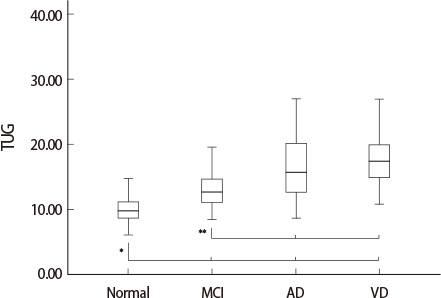
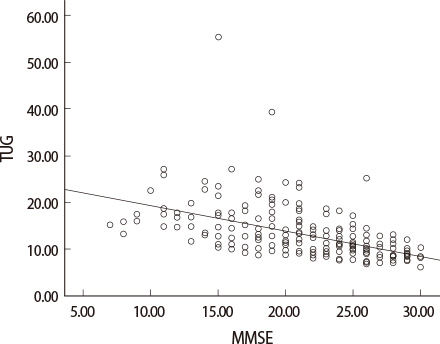
Of the 242 participants, 122 were without cognitive impairment, 51 had mild cognitive impairment, 56 had Alzheimer's disease and 13 had vascular dementia. These four groups showed different results in TUG. Normal group had the lowest values in TUG compare to other groups significantly. MMSE score also correlated with the value of TUG (r=-0.528, p<0.001). Every subcategory of CERAD-K score had significant correlation with the value of TUG. But there were no specific subcategory that had predominant effect in TUG. Only age was an independently significant factor influencing TUG (p<0.05).
CONCLUSIONS
This study shows that increase in age and impairment in cognitive function has an association with gait disturbance. Therefore clinician should be concerned about cognitive factors for evaluation of a patient who has gait disturbance.
MeSH Terms
Figure
Cited by 1 articles
-
Effect of Computerized Neuropsychologic Test in Subacute Post-Stroke Patient With Cognitive Impairment
Chang Hwa Lee, Won Sik Moon, Yong Hyun Han, Po Sung Jun, Gi Hun Hwang, Ho Joong Jung
Kosin Med J. 2018;33(1):51-63. doi: 10.7180/kmj.2018.33.1.51.
Reference
-
1. Snijders AH, Van De Warrenburg BP, Giladi N, Bloem BR. Neurological gait disorders in elderly people: clinical approach and classification. Lancet Neurol. 2007; 6:63–74.
Article2. Sudarsky L. Gait disorders: prevalence, morbidity, and etiology. Adv Neurol. 2001; 87:111–117.
Article3. Verghese J, Lipton RB, Hall CB, Kuslansky G, Katz MJ, Buschke H. Abnormality of gait as a predictor of non-Alzheimer's dementia. N Engl J Med. 2002; 347:1761–1768.
Article4. Bloem B, Gussekloo J, Lagaay A, Remarque E, Haan J, Westendorp R. Idiopathic senile gait disorders are signs of subclinical disease. J Am Geriatr Soc. 2000; 48:1098–1101.
Article5. Marquis S, Moore MM, Howieson DB, Sexton G, Payami H, Kaye JA, et al. Independent predictors of cognitive decline in healthy elderly persons. Arch Neurol. 2002; 59:601.
Article6. Yogev-Seligmann G, Hausdorff JM, Giladi N. The role of executive function and attention in gait. Mov Disord. 2008; 23:329–342.
Article7. Woollacott M, Shumway-Cook A. Attention and the control of posture and gait: a review of an emerging area of research. Gait Posture. 2002; 16:1–14.
Article8. Bland BH, Oddie SD. Theta band oscillation and synchrony in the hippocampal formation and associated structures: the case for its role in sensorimotor integration. Behav Brain Res. 2001; 127:119–136.
Article9. Nutt J, Marsden C, Thompson P. Human walking and higher-level gait disorders, particularly in the elderly. Neurology. 1993; 43:268.
Article10. Podsiadlo D, Richardson S. The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991; 39:142.
Article11. Herman T, Giladi N, Hausdorff JM. Properties of the 'timed up and go' test: more than meets the eye. Gerontology. 2010; 57:203–210.
Article12. Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000; 80:896–903.
Article13. Ku BD, Kim SG, Lee JY, Park KH, Shin JH, Kim KK, et al. Clinical practice guideline for dementia by Clinical Research Center for Dementia of South Korea. J Korean Med Assoc. 2011; 54:861–875.
Article14. Woo JI. The Korean Version of CERAD neuropsychological assessment. 1st ed. Seoul: Seoul National University Press;2010. p. 3–46.
Article15. Jang JS, Kim SK. A Study on The Difference of Memory by the Types of Dementia and Utility of CERAD- K to Vascular Dementia Patients. J Soc Occup Ther Aged Dement. 2012; 6:31–38.
Article16. Jørstad EC, Hauer K, Becker C, Lamb SE. ProFaNE Group. Measuring the psychological outcomes of falling: a systematic review. J Am Geriatr Soc. 2005; 53:501–510.
Article17. Pahapill PA, Lozano AM. The pedunculopontine nucleus and Parkinson's disease. Brain. 2000; 123:1767–1783.
Article18. Nielsen JB. How we walk: central control of muscle activity during human walking. Neuroscientist. 2003; 9:195–204.
Article19. Morton SM, Bastian AJ. Cerebellar control of balance and locomotion. The Neuroscientist. 2004; 10:247–259.
Article20. Gunning-Dixon FM, Raz N. The cognitive correlates of white matter abnormalities in normal aging: a quantitative review. Neuropsychology. 2000; 14:224.
Article21. Giladi N, Herman T, Reider-Groswasser II, Gurevich T, Hausdorff JM. Clinical characteristics of elderly patients with a cautious gait of unknown origin. J Neurol. 2005; 252:300–306.
Article22. Malouin F, Richards CL, Jackson PL, Dumas F, Doyon J. Brain activations during motor imagery of locomotor-related tasks: A PET study. Hum Brain Mapp. 2003; 19:47–62.
Article23. Wiener SI, Berthoz A, Zugaro MB. Multisensory processing in the elaboration of place and head direction responses by limbic system neurons. Brain Res Cogn Brain Res. 2002; 14:75–90.
Article24. Scherder E, Eggermont L, Swaab D, van Heuvelen M, Kamsma Y, de Greef M, et al. Gait in ageing and associated dementias; its relationship with cognition. Neurosci Biobehav Rev. 2007; 31:485–497.
Article25. Erickson C, Barnes C. The neurobiology of memory changes in normal aging. Exp Gerontol. 2003; 38:61–69.
Article26. Pugh KG, Lipsitz LA. The microvascular frontal-subcortical syndrome of aging. Neurobiol Aging. 2002; 23:421–431.
Article27. Mungas D, Harvey D, Reed BR, Jagust WJ, DeCarli C, Beckett L, et al. Longitudinal volumetric MRI change and rate of cognitive decline. Neurology. 2005; 65:565–571.
Article28. Pettersson A, Olsson E, Wahlund L-O. Motor function in subjects with mild cognitive impairment and early Alzheimer's disease. Dement Geriatr Cogn Disord. 2005; 19:299–304.
Article29. Shin JH. Diagnosis of dementia: neuropsychological test. Korean J Fam Med. 2010; 31:253–266.
Article30. Lemke MR, Wendorff T, Mieth B, Buhl K, Linnemann M. Spatiotemporal gait patterns during over ground locomotion in major depression compared with healthy controls. J Psychiatr Res. 2000; 34:227–283.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Gait Patterns in Parkinson's Disease with or without Cognitive Impairment
- Maternally Inherited Diabetes and Deafness Presenting with Memory Impairment and Gait Disturbance
- Correlation of Midbrain Diameter and Gait Disturbance in Patients with Idiopathic Normal Pressure Hydrocephalus
- Gait Disturbance and General Weekness
- Gait Disturbance