Yonsei Med J.
2013 Sep;54(5):1207-1213. 10.3349/ymj.2013.54.5.1207.
Outcomes of Gleason Score < or =8 among High Risk Prostate Cancer Treated with 125I Low Dose Rate Brachytherapy Based Multimodal Therapy
- Affiliations
-
- 1Department of Urology, CHA Bundang Medical Center, CHA University, Seongnam, Korea. bebsuzzang@naver.com
- 2Department of Radiation Oncology, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- 3CHA Cancer Research Center, Seoul, Korea.
- KMID: 1793169
- DOI: http://doi.org/10.3349/ymj.2013.54.5.1207
Abstract
- PURPOSE
To investigate the role of low dose rate (LDR) brachytherapy-based multimodal therapy in high-risk prostate cancer (PCa) and analyze its optimal indications.
MATERIALS AND METHODS
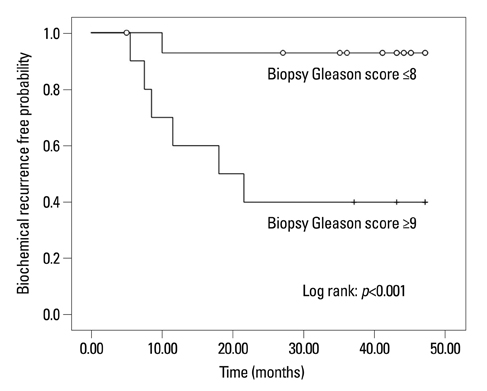
We reviewed the records of 50 high-risk PCa patients [clinical stage > or =T2c, prostate-specific antigen (PSA) >20 ng/mL, or biopsy Gleason score > or =8] who had undergone 125I LDR brachytherapy since April 2007. We excluded those with a follow-up period <3 years. Biochemical recurrence (BCR) followed the Phoenix definition. BCR-free survival rates were compared between the patients with Gleason score > or =9 and Gleason score < or =8.
RESULTS
The mean initial PSA was 22.1 ng/mL, and mean D90 was 244.3 Gy. During a median follow-up of 39.2 months, biochemical control was obtained in 72% (36/50) of the total patients; The estimated 3-year BCR-free survival was 92% for the patients with biopsy Gleason scores < or =8, and 40% for those with Gleason scores > or =9 (p<0.001). In Cox multivariate analysis, only Gleason score > or =9 was observed to be significantly associated with BCR (p=0.021). Acute and late grade > or =3 toxicities were observed in 20% (10/50) and 36% (18/50) patients, respectively.
CONCLUSION
Our results showed that 125I LDR brachytherapy-based multimodal therapy in high-risk PCa produced encouraging relatively long-term results among the Asian population, especially in patients with Gleason score < or =8. Despite small number of subjects, biopsy Gleason score > or =9 was a significant predictor of BCR among high risk PCa patients after brachytherapy.
MeSH Terms
Figure
Reference
-
1. Stamey TA, Caldwell M, McNeal JE, Nolley R, Hemenez M, Downs J. The prostate specific antigen era in the United States is over for prostate cancer: what happened in the last 20 years? J Urol. 2004; 172(4 Pt 1):1297–1301.
Article2. Cooperberg MR, Lubeck DP, Mehta SS, Carroll PR. CaPSURE. Time trends in clinical risk stratification for prostate cancer: implications for outcomes (data from CaPSURE). J Urol. 2003; 170(6 Pt 2):S21–S25.
Article3. Fang LC, Merrick GS, Butler WM, Galbreath RW, Murray BC, Reed JL, et al. High-risk prostate cancer with Gleason score 8-10 and PSA level ≤15 ng/mL treated with permanent interstitial brachytherapy. Int J Radiat Oncol Biol Phys. 2011; 81:992–996.
Article4. Dibiase SJ, Hussain A, Kataria R, Amin P, Bassi S, Dawson N, et al. Long-term results of a prospective, Phase II study of long-term androgen ablation, pelvic radiotherapy, brachytherapy boost, and adjuvant docetaxel in patients with high-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2011; 81:732–736.
Article5. Bolla M, Collette L, Blank L, Warde P, Dubois JB, Mirimanoff RO, et al. Long-term results with immediate androgen suppression and external irradiation in patients with locally advanced prostate cancer (an EORTC study): a phase III randomised trial. Lancet. 2002; 360:103–106.
Article6. Horwitz EM, Bae K, Hanks GE, Porter A, Grignon DJ, Brereton HD, et al. Ten-year follow-up of radiation therapy oncology group protocol 92-02: a phase III trial of the duration of elective androgen deprivation in locally advanced prostate cancer. J Clin Oncol. 2008; 26:2497–2504.
Article7. D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998; 280:969–974.8. Yossepowitch O, Eastham JA. Radical prostatectomy for high-risk prostate cancer. World J Urol. 2008; 26:219–224.
Article9. Yossepowitch O, Eggener SE, Serio AM, Carver BS, Bianco FJ Jr, Scardino PT, et al. Secondary therapy, metastatic progression, and cancer-specific mortality in men with clinically high-risk prostate cancer treated with radical prostatectomy. Eur Urol. 2008; 53:950–959.
Article10. Merrick GS, Butler WM, Wallner KE, Galbreath RW, Allen ZA, Adamovich E. Androgen-deprivation therapy does not impact cause-specific or overall survival after permanent prostate brachytherapy. Int J Radiat Oncol Biol Phys. 2006; 65:669–677.
Article11. Sylvester JE, Grimm PD, Blasko JC, Millar J, Orio PF 3rd, Skoglund S, et al. 15-Year biochemical relapse free survival in clinical Stage T1-T3 prostate cancer following combined external beam radiotherapy and brachytherapy; Seattle experience. Int J Radiat Oncol Biol Phys. 2007; 67:57–64.
Article12. Roach M 3rd, Hanks G, Thames H Jr, Schellhammer P, Shipley WU, Sokol GH, et al. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys. 2006; 65:965–974.
Article13. Yu Y, Anderson LL, Li Z, Mellenberg DE, Nath R, Schell MC, et al. Permanent prostate seed implant brachytherapy: report of the American Association of Physicists in Medicine Task Group No. 64. Med Phys. 1999; 26:2054–2076.
Article14. Salembier C, Lavagnini P, Nickers P, Mangili P, Rijnders A, Polo A, et al. Tumour and target volumes in permanent prostate brachytherapy: a supplement to the ESTRO/EAU/EORTC recommendations on prostate brachytherapy. Radiother Oncol. 2007; 83:3–10.
Article15. Merrick GS, Grimm PD, Sylvester J, Blasko JC, Butler WM, Allen ZA, et al. Initial analysis of Pro-Qura: a multi-institutional database of prostate brachytherapy dosimetry. Brachytherapy. 2007; 6:9–15.
Article16. Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995; 31:1341–1346.
Article17. Fletcher SG, Mills SE, Smolkin ME, Theodorescu D. Case-matched comparison of contemporary radiation therapy to surgery in patients with locally advanced prostate cancer. Int J Radiat Oncol Biol Phys. 2006; 66:1092–1099.
Article18. Stokes SH. Comparison of biochemical disease-free survival of patients with localized carcinoma of the prostate undergoing radical prostatectomy, transperineal ultrasound-guided radioactive seed implantation, or definitive external beam irradiation. Int J Radiat Oncol Biol Phys. 2000; 47:129–136.
Article19. Zelefsky MJ, Hollister T, Raben A, Matthews S, Wallner KE. Five-year biochemical outcome and toxicity with transperineal CT-planned permanent I-125 prostate implantation for patients with localized prostate cancer. Int J Radiat Oncol Biol Phys. 2000; 47:1261–1266.
Article20. Dattoli M, Wallner K, True L, Cash J, Sorace R. Long-term outcomes after treatment with brachytherapy and supplemental conformal radiation for prostate cancer patients having intermediate and high-risk features. Cancer. 2007; 110:551–555.
Article21. Stone NN, Potters L, Davis BJ, Ciezki JP, Zelefsky MJ, Roach M, et al. Multicenter analysis of effect of high biologic effective dose on biochemical failure and survival outcomes in patients with Gleason score 7-10 prostate cancer treated with permanent prostate brachytherapy. Int J Radiat Oncol Biol Phys. 2009; 73:341–346.
Article22. da Silva Franca CA, Vieira SL, Carvalho AC, Bernabé AJ, Penna AB. Localized prostate cancer with intermediate- or high-risk features treated with combined external beam radiotherapy and iodine-125 seed brachytherapy. Brachytherapy. 2010; 9:307–312.
Article23. Tareen B, Kimmel J, Huang WC. Contemporary treatment of high-risk localized prostate cancer. Expert Rev Anticancer Ther. 2010; 10:1069–1076.
Article24. Loeb S, Schaeffer EM, Trock BJ, Epstein JI, Humphreys EB, Walsh PC. What are the outcomes of radical prostatectomy for high-risk prostate cancer? Urology. 2010; 76:710–714.
Article25. Stock RG, Stone NN, Tabert A, Iannuzzi C, DeWyngaert JK. A dose-response study for I-125 prostate implants. Int J Radiat Oncol Biol Phys. 1998; 41:101–108.
Article26. Kao J, Stone NN, Lavaf A, Dumane V, Cesaretti JA, Stock RG. (125)I monotherapy using D90 implant doses of 180 Gy or greater. Int J Radiat Oncol Biol Phys. 2008; 70:96–101.
Article27. Ho AY, Burri RJ, Cesaretti JA, Stone NN, Stock RG. Radiation dose predicts for biochemical control in intermediate-risk prostate cancer patients treated with low-dose-rate brachytherapy. Int J Radiat Oncol Biol Phys. 2009; 75:16–22.
Article28. Schafer JW, Welzel G, Trojan L, Eppler N, Harrer K, Michel MS, et al. Long-term health-related quality-of-life outcomes after permanent prostate brachytherapy. Onkologie. 2008; 31:599–603.
Article29. Koontz BF, Chino J, Lee WR, Hahn CA, Buckley N, Huang S, et al. Morbidity and prostate-specific antigen control of external beam radiation therapy plus low-dose-rate brachytherapy boost for low, intermediate, and high-risk prostate cancer. Brachytherapy. 2009; 8:191–196.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Low-Dose-Rate Brachytherapy for Low- and Intermediate-Risk Groups of Localized Prostate Cancer
- Current Status of Brachytherapy for Prostate Cancer
- Testosterone Replacement Therapy for Patients with Hypogonadism after High Dose-Rate Brachytherapy for High-Risk Prostate Cancer: A Report of Six Cases and Literature Review
- A comparison of preplan MRI and preplan CT-based prostate volume with intraoperative ultrasound-based prostate volume in real-time permanent brachytherapy
- Use of Serum PSA in Comparison of Biopsy Gleason Score with Radical Prostatectomy Gleason Score