Comparative Estimation of Coverage between National Immunization Program Vaccines and Non-NIP Vaccines in Korea
- Affiliations
-
- 1Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea. eunchoi@snu.ac.kr
- 2Department of Preventive Medicine, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 1793041
- DOI: http://doi.org/10.3346/jkms.2013.28.9.1283
Abstract
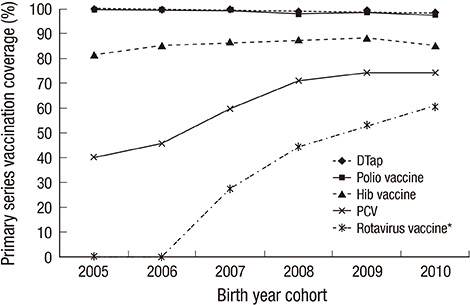
- This study aimed to describe the differences in vaccination coverage between National Immunization Program (NIP) vaccines and non-NIP vaccines in Korea and to identify factors affecting the difference. Nationwide face-to-face interview-based questionnaire survey among randomly selected 4,374 participants aged 7-83 months was conducted. Vaccination coverage analyzed according to the birth cohorts, geographic areas, and socio-demographic characteristics. We found that NIP vaccines recorded higher primary vaccination coverage compared to non-NIP vaccines (95.9%-100% vs 30.7%-85.4%). The highest rate was Haemophilus influenzae type b (Hib) vaccine (85.4%), which was introduced in 1996, and the lowest rate was rotavirus vaccine (30.7%), which was introduced recently. On multivariate analysis, having a sibling were significantly associated with lower uptake of Hib vaccine, pneumococcal conjugate vaccine (PCV), and rotavirus vaccine; while, older mother's age and attendance to daycare center were significantly associated with lower uptake of PCV and rotavirus vaccine (P < 0.001). We found differences in the vaccine coverage rate between NIP vaccines and non-NIP vaccines; and the data suggests potential disparity in accessing non-NIP vaccines in Korea. Expansion of NIP to include non-NIP vaccines can provide better protection against the diseases through increased coverage.
MeSH Terms
-
Adult
Asian Continental Ancestry Group
Child
Child Day Care Centers
Child, Preschool
Cohort Studies
Demography
Female
Haemophilus Infections/prevention & control
Humans
*Immunization Programs
Infant
Interviews as Topic
Male
Multivariate Analysis
Pneumococcal Infections/prevention & control
Questionnaires
Republic of Korea
Rotavirus Infections/prevention & control
Socioeconomic Factors
*Vaccination
Figure
Cited by 11 articles
-
Letter to the Editor: Epidemiological Comments on the Effectiveness of the Varicella Vaccine in Korea
BongKyoo Choi, Ji-hyeun Shin, Jee Eun Lee, Sangbaek Koh
J Korean Med Sci. 2020;35(28):e265. doi: 10.3346/jkms.2020.35.e265.Etiology of Invasive Bacterial Infections in Immunocompetent Children in Korea (2006–2010): a Retrospective Multicenter Study
Kyuyol Rhie, Eun Hwa Choi, Eun Young Cho, Jina Lee, Jin Han Kang, Dong Soo Kim, Yae-Jean Kim, Youngmin Ahn, Byung Wook Eun, Sung Hee Oh, Sung-Ho Cha, Young Jin Hong, Kwang Nam Kim, Nam Hee Kim, Yun-Kyung Kim, Jong-Hyun Kim, Taekjin Lee, Hwang Min Kim, Kun Song Lee, Chun Soo Kim, Su Eun Park, Young Mi Kim, Chi Eun Oh, Sang Hyuk Ma, Dae Sun Jo, Young Youn Choi, Hoan Jong Lee
J Korean Med Sci. 2018;33(6):. doi: 10.3346/jkms.2018.33.e45.Effects of One-dose Varicella Vaccination on Disease Severity in Children during Outbreaks in Seoul, Korea
Young Hwa Lee, Young June Choe, Sung-Il Cho, HyeKyung Park, Ji Hwan Bang, Jong-koo Lee
J Korean Med Sci. 2019;34(10):. doi: 10.3346/jkms.2019.34.e83.Distribution of Human Rotavirus Genotypes in a Tertiary Hospital, Seoul, Korea During 2009-2013
Tae Hee Han, Sang-Hun Park, Ju-Young Chung, Eung-Soo Hwang
Pediatr Infect Vaccine. 2015;22(2):81-90. doi: 10.14776/piv.2015.22.2.81.Post-exposure Prophylaxis against Varicella Zoster Virus in Hospitalized Children after Inadvertent Exposure
Song I Yang, Ji Hee Lim, Eun Jin Kim, Ji Young Park, Ki Wook Yun, Hoan Jong Lee, Eun Hwa Choi
Pediatr Infect Vaccine. 2016;23(3):180-187. doi: 10.14776/piv.2016.23.3.180.Clinical Significance of the Bacille Calmette-Guérin Site Reaction in Kawasaki Disease Patients Aged Less than 18 Months
Sung Hyeon Park, Jeong Jin Yu, Jihye You, Mi Jin Kim, Eun Jung Shin, Hyun Ok Jun, Jae Suk Baek, Young-Hwue Kim, Jae-Kon Ko
Pediatr Infect Vaccine. 2018;25(3):148-155. doi: 10.14776/piv.2018.25.e11.Waning Effectiveness of One-dose Universal Varicella Vaccination in Korea, 2011–2018: a Propensity Score Matched National Population Cohort
Kwan Hong, Sangho Sohn, Young June Choe, Kyuyol Rhie, Joon Kee Lee, Mi Seon Han, Byung Chul Chun, Eun Hwa Choi
J Korean Med Sci. 2021;36(36):e222. doi: 10.3346/jkms.2021.36.e222.High Prevalence of Rotavirus G4P[6] Genotypes among Neonates in Two Korean Hospitals
Jae-Seok Kim, Sung Mi Kim, Hyun Soo Kim
Ann Clin Microbiol. 2017;20(3):63-66. doi: 10.5145/ACM.2021.20.3.63.The Changes in the Outbreak of Rotavirus Gastroenteritis in Children after Introduction of Rotavirus Vaccines: A Retrospective Study at a Tertiary Hospital
Dong Kyu Park, Ju-Young Chung
Korean J Pediatr Infect Dis. 2014;21(3):167-173. doi: 10.14776/kjpid.2014.21.3.167.Changes in the Occurrence of Rotavirus Gastroenteritis before and after the Introduction of Rotavirus Vaccine among Hospitalized Pediatric Patients and Estimates of Rotavirus Vaccine Effectiveness
Jung Min Yoon, Tae Hwan Han, So Won Yoon, Yong Joo Kim, Sung Hee Oh
Pediatr Infect Vaccine. 2018;25(1):26-34. doi: 10.14776/piv.2018.25.1.26.The Molecular Epidemiology of Circulating Group A Rotavirus in Gwangju Metropolitan City, Korea: 2008∼2012
Hye-Young Kee, Min Ji Kim, Sun Hee Kim, Dong-Ryong Ha, Eun Sun Kim, Hye Sook Jeong, Jae Keun Chung, Bong Joo Lee
J Bacteriol Virol. 2014;44(2):197-205. doi: 10.4167/jbv.2014.44.2.197.
Reference
-
1. Lee JK, Choi WS. Immunization policy in Korea. Infect Chemother. 2008; 40:14–23.2. Korea Centers for Disease Control and Prevention. Epidemiology and prevention of vaccine-preventable disease. Osong: Ministry of Health and Welfare;2011. p. 3–38.3. Centers for Disease Control and Prevention (CDC). National and state vaccination coverage among children aged 19-35 months: United States, 2010. MMWR Morb Mortal Wkly Rep. 2011; 60:1157–1163.4. Hug S, Weibel D, Delaporte E, Gervaix A, Heininger U. Comparative coverage of supplementary and universally recommended immunizations in children at 24 months of age. Pediatr Infect Dis J. 2012; 31:217–220.5. The United Nations Children's Fund (UNICEF), Statistics and Monitoring Section. Immunization summary: a statistical reference containing data through 2010. New York: WHO/UNICEF;2012.6. Saitoh A, Okabe N. Current issues with the immunization program in Japan: can we fill the "vaccine gap"? Vaccine. 2012; 30:4752–4756.7. Cho IS. An overview and preparation of Korean pediatrician according to the expansion of national immunization program coverage. Korean J Pediatr. 2008; 51:1275–1281.8. Park B, Lee YK, Cho LY, Go UY, Yang JJ, Ma SH, Choi BY, Lee MS, Lee JS, Choi EH, et al. Estimation of nationwide vaccination coverage and comparison of interview and telephone survey methodology for estimating vaccination status. J Korean Med Sci. 2011; 26:711–719.9. Ategbo S, Ngoungou EB, Koko J, Vierin Y, Zang Ndong CE, Moussavou Mouyama A. Immunization coverage of children aged 0 to 5 years in Libreville (Gabon). Sante. 2010; 20:215–219.10. Centers for Disease Control and Prevention (CDC). National, state, and local area vaccination coverage among children aged 19-35 months: United States, 2009. MMWR Morb Mortal Wkly Rep. 2010; 59:1171–1177.11. Theeten H, Vandermeulen C, Roelants M, Hoppenbrouwers K, Depoorter AM, Van Damme P. Coverage of recommended vaccines in children at 7-8 years of age in Flanders, Belgium. Acta Paediatr. 2009; 98:1307–1312.12. Stockwell MS, Kharbanda EO, Martinez RA, Lara M, Vawdrey D, Natarajan K, Rickert VI. Text4Health: impact of text message reminder-recalls for pediatric and adolescent immunizations. Am J Public Health. 2012; 102:e15–e21.13. Bugenske E, Stokley S, Kennedy A, Dorell C. Middle school vaccination requirements and adolescent vaccination coverage. Pediatrics. 2012; 129:1056–1063.14. Bobo JK, Gale JL, Thapa PB, Wassilak SG. Risk factors for delayed immunization in a random sample of 1163 children from Oregon and Washington. Pediatrics. 1993; 91:308–314.15. Essex C, Smale P, Geddis D. Immunisation status and demographic characteristics of New Zealand infants at 1 year and 2 years of age. N Z Med J. 1995; 108:244–246.16. Lee JH, Cho HK, Kim KH, Kim CH, Kim DS, Kim KN, Cha SH, Oh SH, Hur JK, Kang JH, et al. Etiology of invasive bacterial infections in immunocompetent children in Korea (1996-2005): a retrospective multicenter study. J Korean Med Sci. 2011; 26:174–183.17. Choi EH, Kim SH, Eun BW, Kim SJ, Kim NH, Lee J, Lee HJ. Streptococcus pneumoniae serotype 19A in children, South Korea. Emerg Infect Dis. 2008; 14:275–281.18. Eun BW, Kim SJ, Cho EY, Lee J, Choi EH, Lee HJ. Genetic structure of Streptococcus pneumoniae isolated from children in a tertiary care university hospital, in Korea, 1995 to 2005. Diagn Microbiol Infect Dis. 2010; 68:345–351.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sentinel Safety Monitoring System for Adverse Events of Special Interest Associated With Non-NIP Vaccines in Korea
- Paths toward hepatitis B immunization in South Korea and Taiwan
- An overview and preparation of Korean pediatrician according to the expansion of national immunization program coverage
- Perspectives on vaccine injury compensation program in Korea: the pediatricians' view
- Establishment of Safety Monitoring System for Vaccines Not Included in the National Immunization Program in Korea