J Korean Med Sci.
2010 Apr;25(4):608-612. 10.3346/jkms.2010.25.4.608.
Neuroanatomical Study of Periprostatic Nerve Distributions Using Human Cadaver Prostate
- Affiliations
-
- 1Department of Urology, School of Medicine, Kyung Hee University, Seoul, Korea. sgchang@khu.ac.kr
- 2Department of Pathology, School of Medicine, Kyung Hee University, Seoul, Korea.
- KMID: 1792933
- DOI: http://doi.org/10.3346/jkms.2010.25.4.608
Abstract
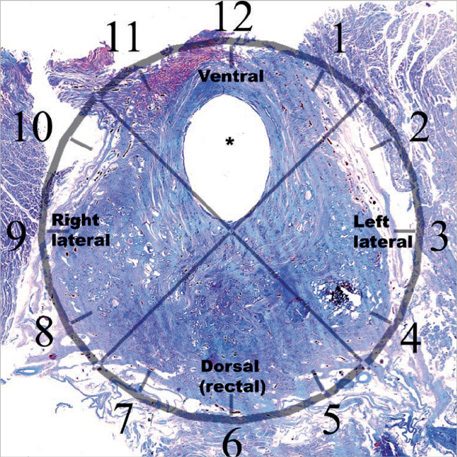
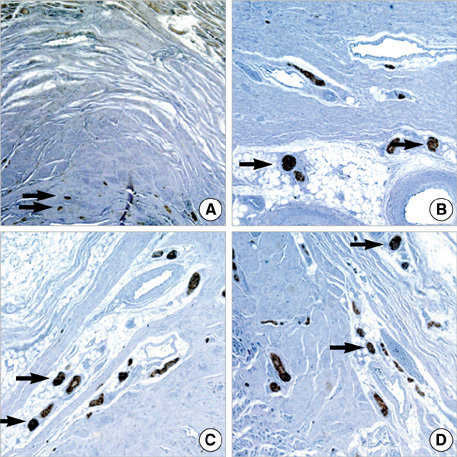
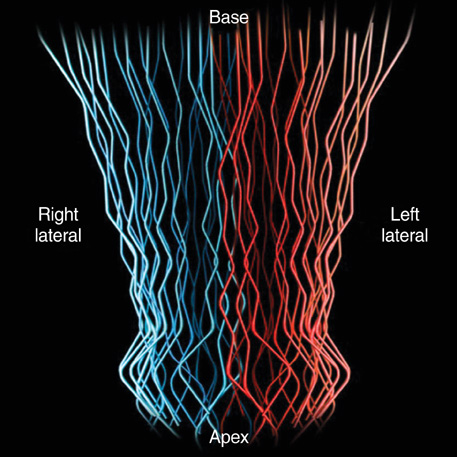
- We investigated the distribution and navigation of periprostatic nerve fibers and constructed a 3-dimensional model of nerve distribution. A total of 5 cadaver specimens were serially sectioned in a transverse direction with 0.5 cm intervals. Hematoxylineosin staining and immunohistochemical staining were then performed on whole-mount sections. Three representative slides from the base, mid-part, and apex of each prostate were subsequently divided into 4 sectors: two lateral, one ventral, and one dorsal (rectal) part. The number of nerve fibers, the distance from nerve fiber to prostate capsule, and the nerve fiber diameters were analyzed on each sector from the representative slides by microscopy. Periprostatic nerve fibers revealed a relatively even distribution in both lateral and dorsal parts of the prostate. There was no difference in the distances from the prostate capsule to nerve fibers. Nerve fibers in the ventral area were also thinner as compared to other areas. In conclusion, periprostatic nerve fibers were observed to be distributed evenly in the periprostatic area, with the exception of the ventral area. As the number of nerve fibers on the ventral part is fewer in comparison, an excessive high up incision is insignificant during the nerve-sparing radical prostatectomy.
MeSH Terms
Figure
Reference
-
1. Augustin H, Hammerer P, Graefen M, Palisaar J, Noldus J, Fernandez S, Huland H. Intraoperative and perioperative morbidity of contemporary radical retropubic prostatectomy in a consecutive series of 1243 patients: results of a single center between 1999 and 2002. Eur Urol. 2003. 43:113–118.
Article2. Graefen M, Walz J, Huland H. Open retropubic nerve-sparing radical prostatectomy. Eur Urol. 2006. 49:38–48.
Article3. Hull GW, Rabbani F, Abbas F, Wheeler TM, Kattan MW, Scardino PT. Cancer control with radical prostatectomy alone in 1,000 consecutive patients. J Urol. 2002. 167:528–534.
Article4. Michl U, Graefen M, Noldus J, Eggert T, Huland H. Functional results of various surgical techniques for radical prostatectomy. Urologe A. 2003. 42:1196–1202.5. Walsh PC, Donker PJ. Impotence following radical prostatectomy: insight into etiology and prevention. J Urol. 1982. 128:492–497.
Article6. Geary ES, Dendinger TE, Freiha FS, Stamey TA. Nerve sparing radical prostatectomy: a different view. J Urol. 1995. 154:145–149.
Article7. Walsh PC, Mostwin JL. Radical prostatectomy and cystoprostatectomy with preservation of potency. Results using a new nerve-sparing technique. Br J Urol. 1984. 56:694–697.
Article8. Hinman F. Prostate and urethral sphincter, Atlas of urosurgical anatomy. 1993. Philadelphia: WB Saunders Co;345.9. Walsh PC. Nerve grafts are rarely necessary and are unlikely to improve sexual function in men undergoing anatomic radical prostatectomy. Urology. 2001. 57:1020–1024.
Article10. Noldus J, Michl U, Graefen M, Haese A, Hammerer P, Huland H. Patient-reported sexual function after nerve-sparing radical retropubic prostatectomy. Eur Urol. 2002. 42:118–124.
Article11. Kim ED, Nath R, Slawin KM, Kadmon D, Miles BJ, Scardino PT. Bilateral nerve grafting during radical retropubic prostatectomy: extended follow-up. Urology. 2001. 58:983–987.
Article12. Takenaka A, Murakami G, Soga H, Han SH, Arai Y, Fujisawa M. Anatomical analysis of the neurovascular bundle supplying penile cavernous tissue to ensure a reliable nerve graft after radical prostatectomy. J Urol. 2004. 172:1032–1035.
Article13. Tewari A, Takenaka A, Mtui E, Horninger W, Peschel R, Bartsch G, Vaughan ED. The proximal neurovascular plate and the tri-zonal neural architecture around the prostate gland: importance in the athermal robotic technique of nerve-sparing prostatectomy. BJU Int. 2006. 98:314–323.
Article14. Kiyoshima K, Yokomizo A, Yoshida T, Tomita K, Yonemasu H, Nakamura M, Oda Y, Naito S, Hasegawa Y. Anatomical features of periprostatic tissue and its surroundings: a histological analysis of 79 radical retropubic prostatectomy specimens. Jpn J Clin Oncol. 2004. 34:463–468.
Article15. Montorsi F, Salonia A, Suardi N, Gallina A, Zanni G, Briganti A, Deho F, Naspro R, Farina E, Rigatti P. Improving the preservation of the urethral sphincter and neurovascular bundles during open radical retropubic prostatectomy. Eur Urol. 2005. 48:938–945.
Article16. Lunacek A, Schwentner C, Fritsch H, Bartsch G, Strasser H. Anatomical radical retropubic prostatectomy: 'curtain dissection' of the neurovascular bundle. BJU Int. 2005. 95:1226–1231.
Article17. Menon M, Tewari A, Peabody J. Vattikuti Institute prostatectomy: technique. J Urol. 2003. 169:2289–2292.
Article18. Menon M, Shrivastava A, Kaul S, Badani KK, Fumo M, Bhandari M, Peabody JO. Vattikuti Institute prostatectomy: contemporary technique and analysis of results. Eur Urol. 2007. 51:648–657.
Article19. Savera AT, Kaul S, Badani K, Stark AT, Shah NL, Menon M. Robotic radical prostatectomy with the "Veil of Aphrodite" technique: histologic evidence of enhanced nerve sparing. Eur Urol. 2006. 49:1065–1073.
Article20. Eichelberg C, Erbersdobler A, Michl U, Schlomm T, Salomon G, Graefen M, Huland H. Nerve distribution along the prostatic capsule. Eur Urol. 2007. 51:105–110.
Article21. Costello AJ, Dowdle B, Namdarian B, Murphy D. Immunohistochemical study of the cavernous nerves in the peri-prostatic region. 2009. In : American Urological Association Annual Meeting 25-30 April 2009; Chicago, Illinois, USA: Elsevier;577–578.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pain during Transrectal Ultrasound-Guided Prostate Biopsy and the Role of Periprostatic Nerve Block: What Radiologists Should Know
- Comparative Evaluation of Periprostatic Nerve Block with and without Intraprostatic Nerve Block in Transrectal Ultrasound-Guided Prostatic Needle Biopsy
- The Effects of Combination Perianal-Intrarectal Lidocaine-Prilocaine Cream and Periprostatic Nerve Block for Pain Control during Transrectal Ultrasound Guided Biopsy of the Prostate: A Randomized, Controlled Trial
- The Effects of Combination of Intrarectal Lidocaine-gel with Periprostatic Lidocaine Injection on the Pain Relief in Repeated Transrectal Prostate Biopsy
- Effect of Periprostatic Nerve Blockade for Transrectal Ultrasound Guided Biopsy of the Prostate