Korean J Gastroenterol.
2009 Jun;53(6):348-354. 10.4166/kjg.2009.53.6.348.
Association of Lower Urinary Tract Symptoms with Irritable Bowel Syndrome in Adult Men : An Internet-based Survey
- Affiliations
-
- 1Seoul National University Hospital Kangnam Center, Seoul, Korea.
- 2Department of Internal Medicine, Seoul National University Boramae Hospital, Seoul, Korea. caskim@brm.co.kr
- 3Department of Urology, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 1792751
- DOI: http://doi.org/10.4166/kjg.2009.53.6.348
Abstract
-
BACKGROUND/AIMS: Patients with irritable bowel syndrome (IBS) are more likely to experience certain urinary symptoms. The aims of this study were to investigate the association between lower urinary tract symptoms (LUTS) and IBS, and to determine their impact on the quality of life.
METHODS
E-mails were sent to 23,594 men who were registered at an internet survey company. Subjects were requested to fill out the questionnaires regarding IBS and LUTS assessed by the International Prostate Symptom Score (IPSS).
RESULTS
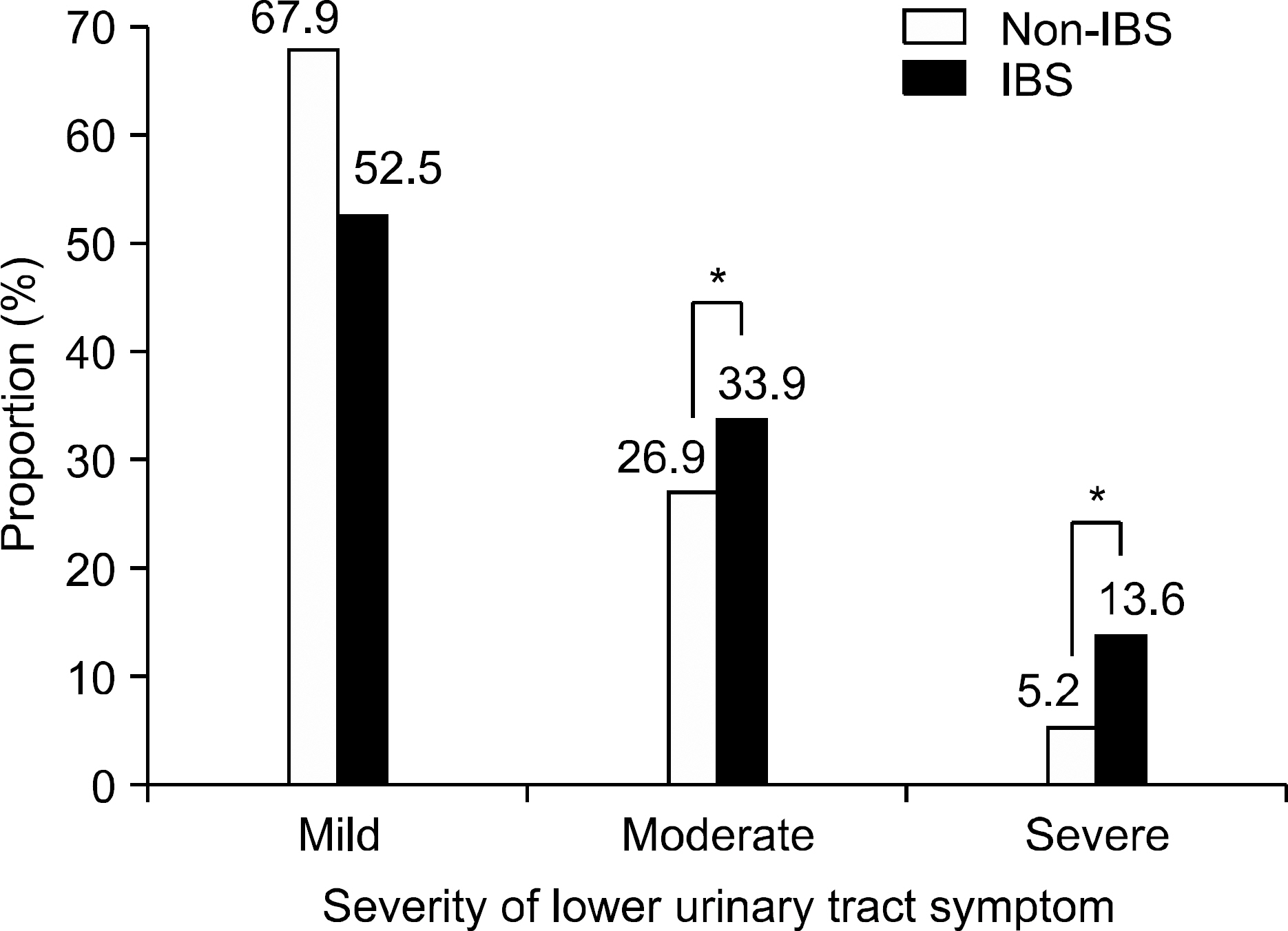
Among 601 subjects (mean age, 35.5+/-8.4) included in the final analysis, 118 (19.6%) fulfilled the Rome II criteria for the diagnosis of IBS. The total mean IPSS of IBS subjects was 9.6, which was significantly higher than the 7.0 of non-IBS subjects (p<0.01). When IPSS was subcategorized into mild, moderate, and severe symptom categories, the proportions with the moderate and severe symptoms among IBS subjects were 33.9% and 13.6% respectively, which were significantly higher than those of non-IBS subjects; (26.9 and 5.2%) (p<0.01). In multivariate analysis, statistically significant association was found between IBS and moderate to severe LUTS (OR, 1.91; 95% CI, 1.27-2.88). IBS subjects also showed a poorer quality of life score than non-IBS subjects (2.24 vs. 1.65, p<0.001).
CONCLUSIONS
LUTS in adult men with IBS are more severe and have a more negative impact on the quality of life than in non-IBS subjects.
MeSH Terms
Figure
Reference
-
1. Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Muller-Lissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999; 45:43–47.
Article2. Rhee PL. Definition and epidemiology of irritable bowel syndrome. Korean J Gastroenterol. 2006; 47:94–100.3. Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006; 130:1480–1491.
Article4. Kim JS, Lee KJ, Kim JH, Hahm KB, Cho SW. Functional gastrointestinal disorders in patients referred to specialist gastroenterologists in a tertiary hospital. Korean J Gastrointest Motil. 2004; 10:111–117.5. Lee SY, Lee KJ, Kim SJ, Cho SW. Prevalence and risk factors for overlaps between gastroesophageal reflux disease, dyspepsia, and irritable bowel syndrome: a population-based study. Digestion. 2009; 79:196–201.
Article6. Ringel Y, Williams RE, Kalilani L, Cook SF. Prevalence, characteristics, and impact of bloating symptoms in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2009; 7:68–72.
Article7. Park JM, Choi MG, Kim YS, et al. Quality of life of patients with irritable bowel syndrome in Korea. Qual Life Res. 2009; 18:435–446.
Article8. Jones R, Latinovic R, Charlton J, Gulliford M. Physical and psychological comorbidity in irritable bowel syndrome: a matched cohort study using the General Practice Research Database. Aliment Pharmacol Ther. 2006; 24:879–886.
Article9. Whitehead WE, Palsson O, Jones KR. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications? Gastroenterology. 2002; 122:1140–1156.
Article10. Walker EA, Gelfand AN, Gelfand MD, Green C, Katon WJ. Chronic pelvic pain and gynecological symptoms in women with irritable bowel syndrome. J Psychosom Obstet Gynaecol. 1996; 17:39–46.
Article11. Vandvik PO, Lydersen S, Farup PG. Prevalence, comorbidity and impact of irritable bowel syndrome in Norway. Scand J Gastroenterol. 2006; 41:650–656.
Article12. Riedl A, Schmidtmann M, Stengel A, et al. Somatic co-morbidities of irritable bowel syndrome: a systematic analysis. J Psychosom Res. 2008; 64:573–582.
Article13. Cukier JM, Cortina-Borja M, Brading AF. A case-control study to examine any association between idiopathic detrusor instability and gastrointestinal tract disorder, and between irritable bowel syndrome and urinary tract disorder. Br J Urol. 1997; 79:865–878.
Article14. Azpiroz F, Dapoigny M, Pace F, et al. Nongastrointestinal disorders in the irritable bowel syndrome. Digestion. 2000; 62:66–72.
Article15. Whorwell PJ, McCallum M, Creed FH, Roberts CT. Non-colonic features of irritable bowel syndrome. Gut. 1986; 27:37–40.
Article16. Francis CY, Duffy JN, Whorwell PJ, Morris J. High prevalence of irritable bowel syndrome in patients attending urological outpatient departments. Dig Dis Sci. 1997; 42:404–407.17. Lee SY, Kim BG, Kim JW, et al. The relationship between irritable bowel syndrome and urinary symptoms in young adult women: an internet survey. Korean J Gastrointest Motil. 2005; 11:44–49.18. Song SH, Jeon H, Kim SW, Paick JS, Son H. The prevalence and risk factors of female sexual dysfunction in young Korean women: an internet-based survey. J Sex Med. 2008; 5:1694–1701.
Article20. Barry MJ, Fowler FJ Jr, O'Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK. Correlation of the American Urological Association symptom index with self-administered versions of the Madsen-Iversen, Boyarsky and Maine Medical Assessment Program symptom indexes. Measurement Com-mittee of the American Urological Association. J Urol. 1992; 148:1558–1563.21. Levy RL, Von Korff M, Whitehead WE, et al. Costs of care for irritable bowel syndrome patients in a health maintenance organization. Am J Gastroenterol. 2001; 96:3122–3129.
Article22. Longstreth GF, Wolde-Tsadik G. Irritable bowel-type symptoms in HMO examinees. Prevalence, demographics, and clinical correlates. Dig Dis Sci. 1993; 38:1581–1589.23. Sperber AD, Carmel S, Atzmon Y, et al. The sense of coher-ence index and the irritable bowel syndrome. A cross-sectional comparison among irritable bowel syndrome patients with and without coexisting fibromyalgia, irritable bowel syndrome non-patients, and controls. Scand J Gastroenterol. 1999; 34:259–263.24. Maxton DG, Morris J, Whorwell PJ. More accurate diagnosis of irritable bowel syndrome by the use of ‘non-colonic' symptomatology. Gut. 1991; 32:784–786.
Article25. Nyhlin H, Ford MJ, Eastwood J, et al. Non-alimentary aspects of the irritable bowel syndrome. J Psychosom Res. 1993; 37:155–162.
Article26. Zimmerman J. Extraintestinal symptoms in irritable bowel syndrome and inflammatory bowel diseases: nature, severity, and relationship to gastrointestinal symptoms. Dig Dis Sci. 2003; 48:743–749.27. Sagnier PP, MacFarlane G, Teillac P, Botto H, Richard F, Boyle P. Impact of symptoms of prostatism on level of both-er and quality of life of men in the French community. J Urol. 1995; 153:669–673.
Article28. Lepor H, Machi G. Comparison of AUA symptom index in unselected males and females between fifty-five and sev-enty-nine years of age. Urology. 1993; 42:36–40.
Article29. Lee WC, Wu CC, Wu HP, Tai TY. Lower urinary tract symptoms and uroflowmetry in women with type 2 diabetes mellitus with and without bladder dysfunction. Urology. 2007; 69:685–690.
Article30. Groutz A, Blaivas JG, Fait G, Sassone AM, Chaikin DC, Gordon D. The significance of the American Urological Association symptom index score in the evaluation of women with bladder outlet obstruction. J Urol. 2000; 163:207–211.
Article31. Monga AK, Marrero JM, Stanton SL, Lemieux MC, Maxwell JD. Is there an irritable bladder in the irritable bowel syndrome? Br J Obstet Gynaecol. 1997; 104:1409–1412.
Article32. Whorwell PJ, Lupton EW, Erduran D, Wilson K. Bladder smooth muscle dysfunction in patients with irritable bowel syndrome. Gut. 1986; 27:1014–1017.
Article33. Chey WY, Jin HO, Lee MH, Sun SW, Lee KY. Colonic mo-tility abnormality in patients with irritable bowel syndrome exhibiting abdominal pain and diarrhea. Am J Gastroenterol. 2001; 96:1499–1506.
Article34. Malykhina AP, Qin C, Greenwood-van Meerveld B, Foreman RD, Lupu F, Akbarali HI. Hyperexcitability of convergent colon and bladder dorsal root ganglion neurons after colonic inflammation: mechanism for pelvic organ cross-talk. Neurogastroenterol Motil. 2006; 18:936–948.
Article35. Qin C, Malykhina AP, Akbarali HI, Foreman RD. Cross-or-gan sensitization of lumbosacral spinal neurons receiving urinary bladder input in rats with inflamed colon. Gastroenterology. 2005; 129:1967–1978.
Article36. Han SH, Lee OY, Bae SC, et al. Prevalence of irritable bowel syndrome in Korea: population-based survey using the Rome II criteria. J Gastroenterol Hepatol. 2006; 21:1687–1692.
Article37. Park KS, Ahn SH, Hwang JS, et al. A survey about irritable bowel syndrome in South Korea: prevalence and observable organic abnormalities in IBS patients. Dig Dis Sci. 2008; 53:704–711.38. Pequegnat W, Rosser BR, Bowen AM, et al. Conducting internet-based HIV/STD prevention survey research: consid-erations in design and evaluation. AIDS Behav. 2007; 11:505–521.
Article39. Fortson BL, Scotti JR, Del Ben KS, Chen YC. Reliability and validity of an Internet traumatic stress survey with a college student sample. J Trauma Stress. 2006; 19:709–720.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Relationship between Irritable Bowel Syndrome and Urinary Symptoms in Young Adult Women: an Internet Survey
- Irritable Bowel Syndrome Is More Common in Women Regardless of the Menstrual Phase: A Rome II-based Survey
- The Urinary Tract Microbiome in Male Genitourinary Diseases: Focusing on Benign Prostate Hyperplasia and Lower Urinary Tract Symptoms
- Irritable bowel syndrome
- Decreased Neuroplasticity May Play a Role in Irritable Bowel Syndrome: Implication From the Comorbidity of Depression and Irritable Bowel Syndrome