J Korean Med Sci.
2008 Jun;23(3):390-396. 10.3346/jkms.2008.23.3.390.
Atopy May Be an Important Determinant of Subepithelial Fibrosis in Subjects with Asymptomatic Airway Hyperresponsiveness
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. shcho@plaza.snu.ac.kr
- 2Institute of Allergy and Clinical Immunology, Seoul National University Medical Research Center, Seoul, Korea.
- 3Department of Internal Medicine, Dongguk University International Hospital, Goyang, Korea.
- 4Department of Internal Medicine, Seoul National University Bundang Hospitial, Seongnam, Korea.
- 5Department of Pathology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 6Department of Pathology, Seoul National University Hospital, Seoul, Korea.
- 7Department of Life Science, Pohang Biotechnology Center, Pohang University of Science and Technology, Pohang, Korea.
- KMID: 1786874
- DOI: http://doi.org/10.3346/jkms.2008.23.3.390
Abstract
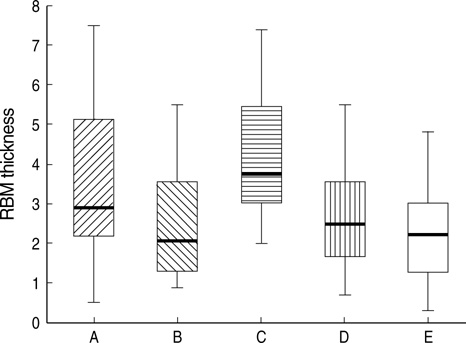
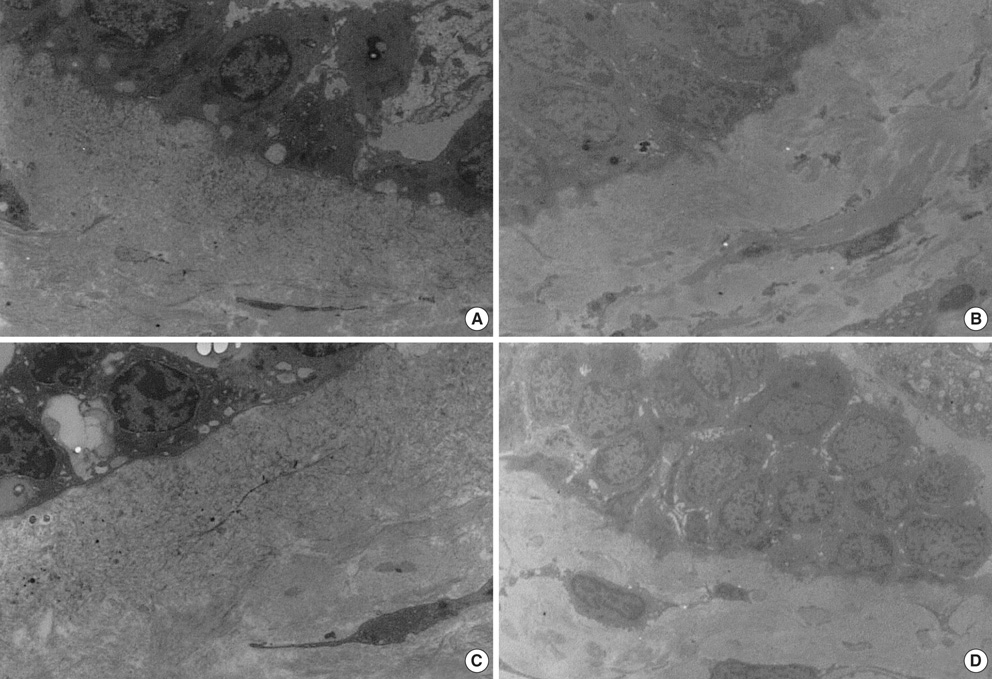
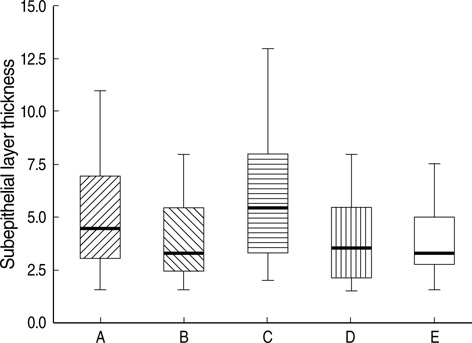
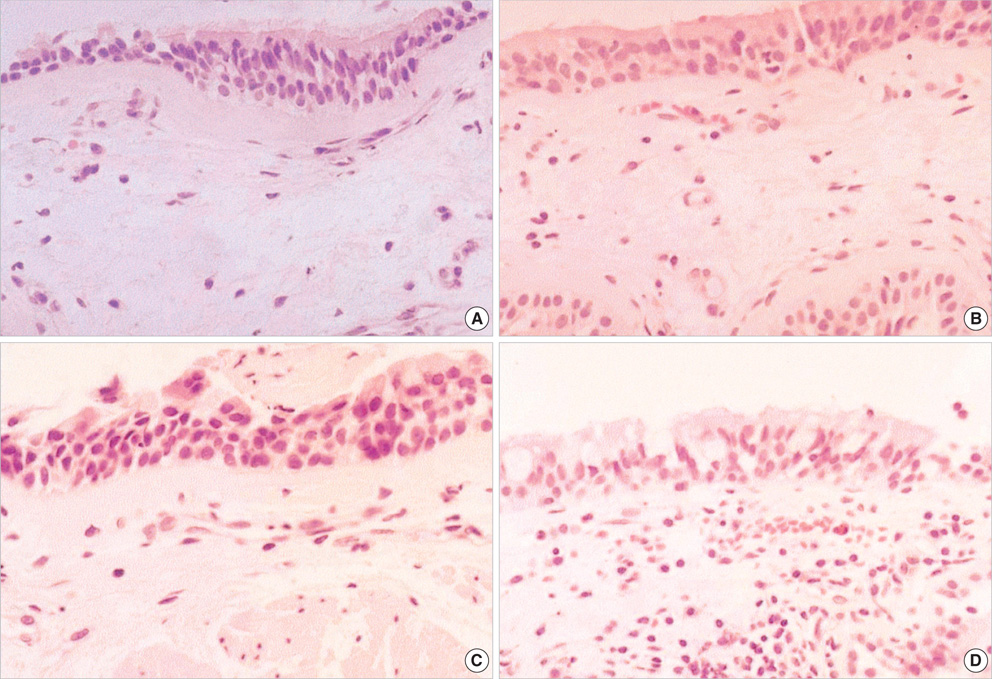
- The bronchial pathology of asymptomatic airway hyperreponsiveness (AHR) subjects is not well understood, and the role of atopy in the development of airway remodeling is unclear. The aim of this study was to evaluate whether atopy is associated with airway remodeling in asymptomatic AHR subjects. Five groups, i.e., atopic or non-atopic subjects with asymptomatic AHR, atopic or non-atopic healthy controls, and subjects with mild atopic asthma, were evaluated by bronchoscopic biopsy. By electron microscopy, mean reticular basement membrane (RBM) thicknesses were 4.3+/-1.7 micrometer, 3.4+/-1.8 micrometer, 2.5+/-1.5 micrometer, 2.6+/-1.1 micrometer, and 2.3+/-1.2 micrometer in the mild atopic asthma, atopic and non-atopic asymptomatic AHR, atopic and nonatopic control groups, respectively (p=0.002). RBM thicknesses were significantly higher in the mild atopic asthma group and in the atopic asymptomatic AHR group than in the other three groups (p=0.048). No significant difference in RBM thickness was observed between the atopic asymptomatic AHR group and the mild atopic asthma group (p>0.05), nor between non-atopic asymptomatic AHR group and the two control groups (p>0.05). By light microscopy, subepithelial layer thicknesses between the groups showed the same results. These findings suggest that RBM thickening occurs in subjects with atopic asymptomatic AHR, and that atopy plays an important role in airway remodeling.
Keyword
MeSH Terms
-
Adult
Asthma/epidemiology/*pathology
Basement Membrane/*pathology/ultrastructure
Biopsy
Bronchi/pathology
Bronchial Hyperreactivity/epidemiology/*pathology
Bronchoscopy
Female
Fibrosis
Follow-Up Studies
Humans
Hypersensitivity, Immediate/*epidemiology
Male
Microscopy, Electron
Respiratory Mucosa/*pathology/ultrastructure
Risk Factors
Figure
Reference
-
1. Boulet LP. Asymptomatic airway hyperresponsiveness: a curiosity or an opportunity to prevent asthma? Am J Respir Crit Care Med. 2003; 167:371–378.2. Jansen DF, Timens W, Kraan J, Rijcken B, Postma DS. (A)symptomatic bronchial hyper-responsiveness and asthma. Respir Med. 1997; 91:121–134.
Article3. Kim YK, Kim SH, Tak YJ, Jee YK, Lee BJ, Kim SH, Park HW, Jung JW, Bahn JW, Chang YS, Choi DC, Chang SI, Min KU, Kim YY, Cho SH. High prevalence of current asthma and active smoking effect among the elderly. Clin Exp Allergy. 2002; 32:1706–1712.
Article4. Laprise C, Laviolette M, Boutet M, Boulet LP. Asymptomatic airway hyperresponsiveness: relationships with airway inflammation and remodelling. Eur Respir J. 1999; 14:63–73.
Article5. Boulet LP, Prince P, Turcotte H, Lemiere C, Olivenstein R, Laprise C, Larivee P, Begin P, Laviolette M. Clinical features and airway inflammation in mild asthma versus asymptomatic airway hyperresponsiveness. Respir Med. 2006; 100:292–299.
Article6. Braunstahl GJ, Fokkens WJ, Overbeek SE, KleinJan A, Hoogsteden HC, Prins JB. Mucosal and systemic inflammatory changes in allergic rhinitis and asthma: a comparison between upper and lower airways. Clin Exp Allergy. 2003; 33:579–587.
Article7. Milanese M, Crimi E, Scordamaglia A, Riccio A, Pellegrino R, Canonica GW, Brusasco V. On the functional consequences of bronchial basement membrane thickening. J Appl Physiol. 2001; 91:1035–1040.
Article8. Amin K, Ludviksdottir D, Janson C, Nettelbladt O, Bjornsson E, Roomans GM, Boman G, Seveus L, Venge P. Inflammation and structural changes in the airways of patients with atopic and nonatopic asthma. Am J Respir Crit Care Med. 2000; 162:2295–2301.
Article9. Laprise C, Boulet LP. Asymptomatic airway hyperresponsiveness: a three-year follow-up. Am J Respir Crit Care Med. 1997; 156:403–409.
Article10. Rasmussen F, Taylor DR, Flannery EM, Cowan JO, Greene JM, Herbison GP, Sears MR. Outcome in adulthood of asymptomatic airway hyperresponsiveness in childhood: a longitudinal population study. Pediatr Pulmonol. 2002; 34:164–171.
Article11. Kerkhof M, Schouten JP, De Monchy JG. The association of sensitization to inhalant allergens with allergy symptoms: the influence of bronchial hyperresponsiveness and blood eosinophil count. Clin Exp Allergy. 2000; 30:1387–1394.
Article12. American Thoracic Society. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease (COPD) and asthma. Am Rev Respir Dis. 1987; 136:225–244.13. Kim YK, Chang YS, Lee MH, Hong SC, Bae JM, Jee YK, Chun BR, Cho SH, Min KU, Kim YY. Role of environmental exposure to spider mites in the sensitization and the clinical manifestation of asthma and rhinitis in children and adolescents living in rural and urban areas. Clin Exp Allergy. 2002; 32:1305–1309.
Article14. Kim YK, Park HS, Kim HY, Jee YK, Son JW, Bae JM, Lee MH, Cho SH, Min KU, Kim YY. Citrus red mite (Panonychus citri) may be an important allergen in the development of asthma among exposed children. Clin Exp Allergy. 2001; 31:582–589.
Article15. American Thoracic Society. Medical section of the American lung association. Guidelines for fiberoptic bronchoscopy in adults. Am Rev Respir Dis. 1987; 136:1066.16. Park SH, Kim MK, Kim H, Song BJ, Chi JG. Ultrastructural studies of gastrointestinal stromal tumors. J Korean Med Sci. 2004; 19:234–244.
Article17. Gray L, Peat JK, Belousova E, Xuan W, Woolcock AJ. Family patterns of asthma, atopy and airway hyperresponsiveness: an epidemiological study. Clin Exp Allergy. 2000; 30:393–399.
Article18. Davies DE, Wicks J, Powell RM, Puddicombe SM, Holgate ST. Airway remodeling in asthma: new insights. J Allergy Clin Immunol. 2003; 111:215–225.19. Rasmussen F, Lambrechtsen J, Siersted HC, Hansen HS, Hansen NC. Asymptomatic bronchial hyperresponsiveness to exercise in childhood and the development of asthma related symptoms in young adulthood: the odense schoolchild study. Thorax. 1999; 54:587–589.
Article20. Xuan W, Peat JK, Toelle BG, Marks GB, Berry G, Woolcock AJ. Lung function growth and its relation to airway hyperresponsiveness and recent wheeze. Results from a longitudinal population study. Am J Respir Crit Care Med. 2000; 161:1820–1824.21. Lange P, Parner J, Vestbo J, Schnohr P, Jensen G. A 15-year follow-up study of ventilatory function in adults with asthma. N Engl J Med. 1998; 339:1194–1200.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship Between Atopy and Bronchial Hyperresponsiveness
- Relationship of serum IL-13 and eotaxin level with airway hyperresponsiveness in children with asthma
- Volatile Organic Compounds Contribute to Airway Hyperresponsiveness
- Airways are More Reactive to Histamine than to Methacholine in Patients with Mild Airway Hyperresponsiveness, Regardless of Atopy
- Effects of CpG-oligodeoxynucleotides in Chronic Inflammation and Remodeling of Airway in a Murine Model of Bronchial Asthma