J Korean Med Sci.
2008 Feb;23(1):94-97. 10.3346/jkms.2008.23.1.94.
Granulocyte Macrophage Colony-Stimulating Factor May Modulate the Post-transcription Pathway of Interleukin-6 Expression in Prostate Carcinoma Cells
- Affiliations
-
- 1Department of Urology, College of Medicine, Chung-Ang University, Seoul, Korea. kthlmk@hanafos.com
- 2Department of Laboratory Medicine, College of Medicine, Chung-Ang University, Seoul, Korea.
- 3Center for Disease Control & Prevention, Seoul, Korea.
- KMID: 1786852
- DOI: http://doi.org/10.3346/jkms.2008.23.1.94
Abstract
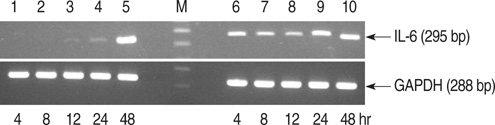
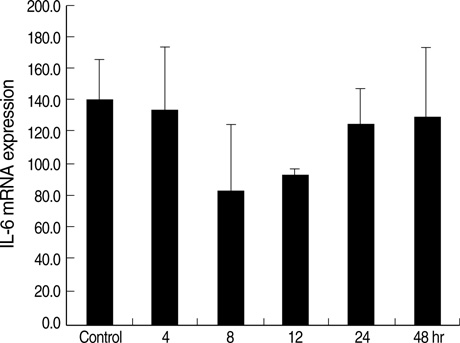
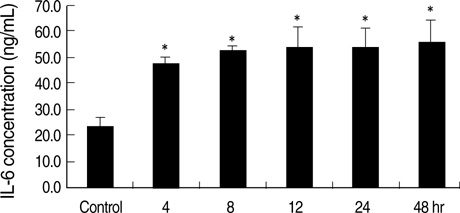
- Interleukin-6 (IL-6) can stimulate a variety of tumors including prostatic carcinoma. Research has recently shown that IL-6 may act to stimulate the progression of prostatic cancer. To date, little research has been performed to better understand the nature of granulocyte macrophage colony-stimulating factor (GM-CSF) and the expression of IL-6. The aim of this study was to evaluate the effects of GM-CSF on the expression of IL-6 in prostate cancer-3 (PC-3) cells. The bone-derived PC-3 cell line was used in this study. Reverse transcription polymerase chain reaction (RT-PCR) and real- time PCR were performed to detect IL-6 mRNA expression. The IL-6 protein was measured by enzyme-linked immunosorbent assay (ELISA) after treatment with hGM-CSF. Our data indicated that IL-6 mRNA expression did not increase after treatment with hGM-CSF in comparison to the control group. However, the expression of IL-6 protein was increased compared to the control group. GM-CSF may modulate the post-transcription pathway of IL-6 expression in prostate carcinoma cells. Our data suggest that GM-CSF may have a role in IL-6-mediated development of prostate cancer.
MeSH Terms
Figure
Reference
-
1. National Statistical office. Republic of Korea. Korea Statistical Information System. Dec., 31, 2002. Available from: URL:http://kosis.nso.go.kr.2. Akira S, Taga T, Kishimoto T. Interleukin-6 in biology and medicine. Adv Immunol. 1993. 54:1–78.
Article3. Tan D, Wu X, Hou M, Lee SO, Lou W, Wang J, Janarthan B, Nallapareddy S, Trump DL, Gao AC. Interleukin-6 polymorphism is associated with more aggressive prostate cancer. J Urol. 2005. 174:753–756.
Article4. Chung TD, Yu JJ, Spiotto MT, Bartkowski M, Simons JW. Characterization of the role of IL-6 in the progression of prostate cancer. Prostate. 1999. 38:199–207.
Article5. Offner FA, Obrist P, Stadlmann S, Feichtinger H, Klingler P, Herold M, Zwierzina H, Hittmair A, Mikuz G, Abendstein B, Zeimet A, Marth C. IL-6 secretion by human peritoneal mesothelial and ovarian cancer cells. Cytokine. 1995. 7:542–547.
Article6. Lee SO, Lou W, Hou M, de Miguel F, Gerber L, Gao AC. Interleukin-6 promotes androgen-independent growth in LNCaP human prostate cancer cells. Clin Cancer Res. 2003. 9:370–376.7. Horwood NJ, Udagawa N, Elliott J, Grail D, Okamura H, Kurimoto M, Dunn AR, Martin T, Gillespie MT. Interleukin 18 inhibits osteoclast formation via T cell production of granulocyte macrophage colony-stimulating factor. J Clin Invest. 1998. 101:595–603.
Article8. Savarese DM, Valinski H, Quesenberry P, Savarese T. Expression and function of colony-stimulating factors and their receptors in human prostate carcinoma cell lines. Prostate. 1998. 34:80–91.
Article9. Small EJ, Reese DM, Um B, Whisenant S, Dixon SC, Figg WD. Therapy of advanced prostate cancer with granulocyte macrophage colony-stimulating factor. Clin Cancer Res. 1999. 5:1738–1744.10. Rini BI, Weinberg V, Bok R, Small EJ. Prostate-specific antigen kinetics as a measure of the biologic effect of granulocyte-macrophage colony-stimulating factor in patients with serologic progression of prostate cancer. J Clin Oncol. 2003. 21:99–105.
Article11. Kim TH, Kim YS, Myung SC, Lee DH, Won EH, Lee SY. The prostaglandin E receptor agonists increase granulocyte macrophage colony-stimulating factor in prostate cancer cells. Korean J Urol. 2004. 45:1272–1278.12. Nakata H, Uemura Y, Kobayashi M, Harada R, Taguchi H. Cyclooxygenase-2 inhibitor NS-398 suppresses cell growth and constitutive production of granulocyte-colony stimulating factor and granulocyte macrophage-colony stimulating factor in lung cancer cells. Cancer Sci. 2003. 94:173–180.
Article13. Guillaume T, Sekhavat M, Rubinstein DB, Hamdan O, Symann ML. Transcription of genes encoding granulocyte-macrophage colony-stimulating factor, interleukin 3, and interleukin 6 receptors and lack of proliferative response to exogenous cytokines in nonhematopoietic human malignant cell lines. Cancer Res. 1993. 53:3139–3144.14. Rokhlin OW, Griebling TL, Karassina NV, Raines MA, Cohen MB. Human prostate carcinoma cell lines secrete GM-CSF and express GM-CSF-receptor on their cell surface. Anticancer Res. 1996. 16:557–563.15. Markowicz S, Engleman EG. Granulocyte-macrophage-colony stimulating factor promotes differentiation and survival of human peripheral blood dendritic cells in vitro. J Clin Invest. 1990. 85:955–961.16. Culig Z. Interleukin-6 polymorphism: expression and pleiotropic regulation in human prostate cancer. J Urol. 2005. 174:417.
Article17. Nakashima J, Tachibana M, Horiguchi Y, Oya M, Ohigashi T, Asakura H, Murai M. Serum interleukin 6 as a prognostic factor in patients with prostate cancer. Clin Cancer Res. 2000. 6:2702–2706.18. Drachenberg DE, Elgamal AA, Rowbotham R, Peterson M, Murphy GP. Circulating levels of interleukin-6 in patients with hormone refractory prostate cancer. Prostate. 1999. 41:127–133.
Article19. Adler HL, McCurdy MA, Kattan MW, Timme TL, Scardino PT, Thompson TC. Elevated levels of circulating interleukin-6 and transforming growth factor-beta1 in patients with metastatic prostate carcinoma. J Urol. 1999. 161:182–187.20. Okamoto M, Lee C, Oyasu R. Interleukin-6 as a paracrine and autocrine growth factor in human prostatic carcinoma cells in vitro. Cancer Res. 1997. 57:141–146.21. Siegall CB, Schwab G, Nordan RP, FitzGerald DJ, Pastan I. Expression of the interleukin-6 receptor and interleukin-6 in prostate carcinoma cells. Cancer Res. 1990. 50:7786–7788.22. Ivanovic V, Melman A, Davis-Joseph B, Valcic M, Geliebter J. Elevated plasma levels of TGF-beta 1 in patients with invasive prostate cancer. Nat Med. 1995. 1:282–284.23. Charyulu VI, Lopez DM. Elevated GM-CSF levels in tumor bearing mice upregulate IL-6 production by B cells via a mechanism independent of TNF-alpha. Int J Oncol. 2000. 16:161–167.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Granulocyte Macrophage Colony-Stimulating Factor (GM-CSF) on the Interleukin-6 Expression in the Prostate Cancer Cell Line PC-3
- The effects on the production of platelet activating factor in the cultured human endothelial cells by interleukin-6 and granulocyte macrophage colony stimulating factor
- The Prostaglandin E Receptor Agonists Increase Granulocyte Macrophage Colony-Stimulating Factor in Prostate Cancer Cells
- Effect of combination gene therapy with herpes simplex virus thymidine kinase suicidal gene and granulocyte-macrophage colony-stimulating factor gene in murine melanoma model
- Cooperative effect of Alternaria and rhinovirus on the activation of nasal polyp epithelial cells