Yonsei Med J.
2007 Dec;48(6):955-962. 10.3349/ymj.2007.48.6.955.
Conjunctival Expansion Using a Subtenon's Silicone Implant in New Zealand White Rabbits
- Affiliations
-
- 1Department of Ophthalmology, Wonju Christian Hospital, Yonsei University, Wonju College of Medicine, Wonju, Korea. shrah@wonju.yonsei.ac.kr
- KMID: 1786209
- DOI: http://doi.org/10.3349/ymj.2007.48.6.955
Abstract
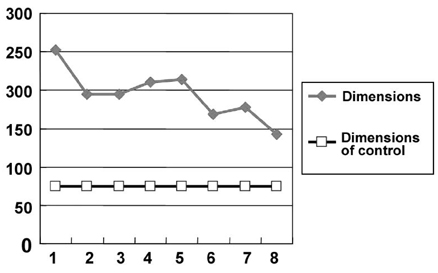
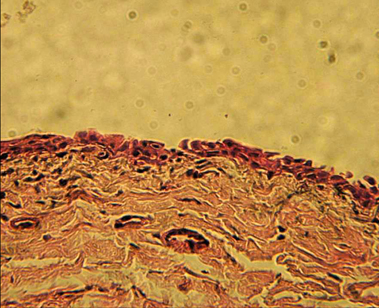
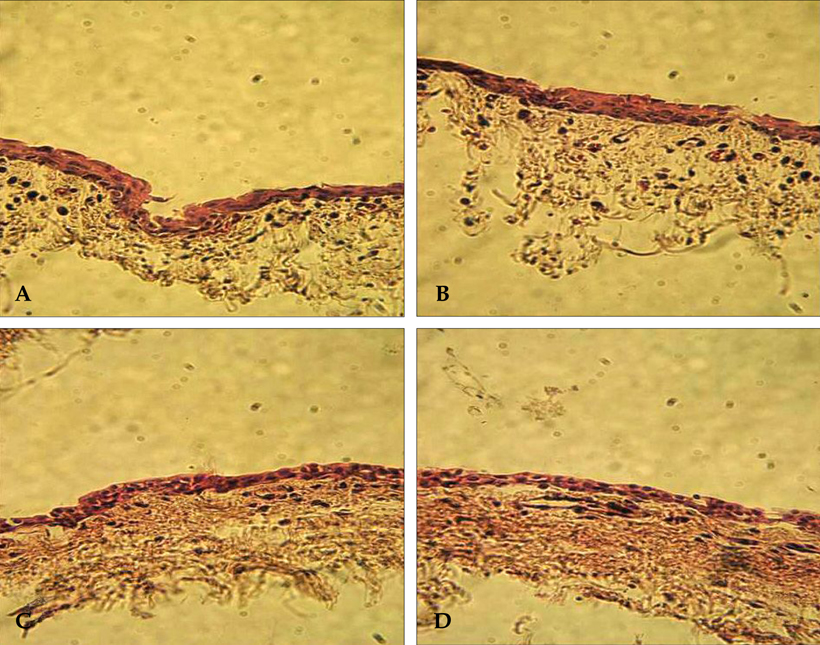
- PURPOSE: In the field of ophthalmology, the conjunctival autograft is a useful therapeutic material in many cases, but the small size of the autograft is a disadvantage. Therefore, we evaluated the feasibility of taking an expanded sample of conjunctival tissue using a subtenon's silicone implant. MATERIALS AND METHODS: We included a total of nine rabbits; eight rabbits were operative cases, and one was a control. A portion of conjunctival tissue from the control rabbit, which did not undergo surgery, was dissected and examined to determine whether it was histologically different from the experimental group. The surgical procedure was performed on eight rabbits via a subtenon's insertion of a silicone sponge in the left superior-temporal portion; after surgery, we dropped antibiotics into the eyes. We sacrificed a pair of rabbits every three days (on days 3, 6, 9, and 12) after surgery, removed the expanded conjunctival tissues with the silicone sponge implants, and measured their sizes. RESULTS: The mean size of the expanded conjunctival tissues was 194.4mm(2). On the third day, we were able to harvest a 223.56mm(2) section of conjunctival tissue, which was the most expanded sample of tissue in the study. On the twelfth day, we removed a 160.38mm(2) section of conjunctival tissue, which was the least expanded sample of tissue. Statistically, there were no significant differences in the mean dimensions of the expanded conjunctival tissues for each time period. Microscopic examinations showed no histological differences between the expanded conjunctival tissues and the normal conjunctival tissues. CONCLUSION: The results reveal that this procedure is a useful method to expand the conjunctiva for grafting and transplantation.
MeSH Terms
Figure
Reference
-
1. Lee SB, Cho YJ, Hahn DK. Clinical experience of conjunctival flaps for persistent ulcerative keratitis. J Korean Ophthalmol Soc. 1996. 37:36–44.2. Brown DD, McCulley JP, Bowman RW, Halsted MA. The use of conjunctival flaps in the treatment of herpes keratouveitis. Cornea. 1992. 11:44–46.
Article3. Lugo M, Arentsen JJ. Treatment of neurotrophic ulcers with conjunctival flaps. Am J Ophthalmol. 1987. 103:711–712.
Article4. Lukáts O. Contracted anophthalmic socket repair. Orbit. 2002. 21:125–130.5. Suh IS, Yang YM, Oh SJ. Conjunctival cul-de-sac reconstruction with radial forearm free flap in anophthalmic orbit syndrome. Plast Reconstr Surg. 2001. 107:914–919.
Article6. Shore JW, McCord CD Jr, Bergin DJ, Dittmar SJ, Maiorca JP, Burks WR. Management of complications following dermis-fat grafting for anophthalmic socket reconstruction. Ophthalmology. 1985. 92:1342–1350.
Article7. Wiese KG, Vogel M, Guthoff R, Gundlach KK. Treatment of congenital anophthalmos with self-inflating polymer expanders: a new method. J Craniomaxillofac Surg. 1999. 27:72–76.
Article8. Mazzoli RA, Raymond WR 4th, Ainbinder DJ, Hansen EA. Use of self-expanding, hydrophilic osmotic expanders (hydrogel) in the reconstruction of congenital cilinical anophthalmos. Curr Opin Ophthalmol. 2004. 15:426–431.
Article9. Eppley BL, Holley S, Sadove AM. Experimental effects of intraorbital tissue expansion on orbitomaxillary growth in anophthalmos. Ann Plast Surg. 1993. 31:19–27.
Article10. Dunaway DJ, David DJ. Intraorbital tissue expansion in the management of congenital anophthalmos. Br J Plast Surg. 1996. 49:529–535.
Article11. Lee YH, Kim HC, Lee JS, Park WJ. Surgical reconstruction of the contracted orbit. Plast Reconstr Surg. 1999. 103:1129–1138.
Article12. Wieslander JB, Wieslander M. Prefabricated (expander) capsule-lined transposition and advancement flaps in reconstruction of lower eyelid and oral defects: an experimental study. Plast Reconstr Surg. 2000. 105:1399–1407.
Article13. Ang LP, Tan DT, Cajucom-Uy H, Beuerman RW. Autologous cultivated conjunctival transplantation for pterygium surgery. Am J Ophthalmol. 2005. 139:611–619.
Article14. Zemba M, Bobeico V, Brătulescu M, Ciucă C, Andrei S, Anton O. Conjunctival autoplasty in pterygium treatment. Oftalmologia. 2005. 49:41–45.15. Uy HS, Reyes JM, Flores JD, Lim-Bon-Siong R. Comparison of fibrin glue and sutures for attaching conjunctival autografts after pterygium excision. Ophthalmology. 2005. 112:667–671.
Article16. Oh TH, Choi KY, Yoon BJ. The effect of conjunctival autograft for recurrent pterygium. J Korean Ophthalmol Soc. 1994. 35:1335–1339.17. Lee CO, Jong SH, Lee JJ. Autologous simple conjunctival graft and conjunctiva/Tenon graft of focal scleromalacia. J Korean Ophthalmol Soc. 1997. 38:1737–1741.18. Kim MJ, Tchah HW. Treatment of pterygium with amniotic membrane transplantation. J Korean Ophthalmol Soc. 1998. 39:59–64.19. Youngson RM. Recurrence of pterygium after excision. Br J Ophthalmol. 1972. 56:120–125.
Article20. Jaros PA, DeLuise VP. Pingueculae and pterygia. Surv Ophthalmol. 1988. 32:41–49.
Article21. Kenyon KR, Wagoner MD, Hettinger ME. Conjunctival autograft transplantation for advanced and recurrent pterygium. Ophthalmology. 1985. 92:1461–1470.
Article22. Riordan-Eva P, Kielhorn I, Ficker LA, Steele AD, Kirkness CM. Conjunctival autografting in the surgical management of pterygium. Eye. 1993. 7:634–638.
Article23. Allan BD, Short P, Crawford GJ, Barrett GD, Constable IJ. Pterygium excision with conjunctival autografting: an effective and safe technique. Br J Ophthalmol. 1993. 77:698–701.
Article24. McCoombes J, Hirst LW, Isbell GP, editors. Recurrence rate following simple excision and sliding conjunctival flap for primary pterygium. 1992. 1992 Nov; Sydney, Australia. Presented at the Annual Scientific Congress of the Royal Australian College of Ophthalmologists.25. Huang Y, Li H, Huang Z, Lin J, Chen J, Li H. Application of amnion membrane transplantation combine with mitomycin C in the treatment of pterygium. Yan Ke Xue Bao. 2004. 20:74–76.26. Fournier JH, McLachlan DL. Ocular surface reconstruction using amniotic membrane allograft for severe surface disorders in chemical burns: case report and review of the literature. Int Surg. 2005. 90:45–47.27. Gündüz K, Uçakhan OO, Kanpolat A, Günalp I. Nonpreserved human amniotic membrane transplantation for conjunctival reconstruction after excision of extensive ocular surface neoplasia. Eye. 2006. 20:351–357.
Article28. Hick S, Demers PE, Brunette I, La C, Mabon M, Duchesne B. Amniotic membrane transplatation and fibrin glue in the management of corneal ulcers and perforations: a review of 33 cases. Cornea. 2005. 24:369–377.
Article29. Lambiase A, Sacchetti M, Sgrulletta R, Coassin M, Bonini S. Amniotic membrane transplantation associated with conjunctival peritomy in the management of Mooren's ulcer: a case report. Eur J Ophthalmol. 2005. 15:274–276.
Article30. Tosi GM, Traversi C, Schuerfeld K, Mittica V, Massaro-Giordano M, Tilanus MA, et al. Amniotic membrane graft: histopathological findings in five cases. J Cell Physiol. 2005. 202:852–857.
Article31. Takano Y, Fukagawa K, Miyake-Kashima M, Tanaka M, Asano-Kato N, Dogru M, et al. Dramatic healing of an allergic corneal ulcer persistent for 6 months by amniotic membrane patching in a patient with atopic keratoconjunctivitis: a case report. Cornea. 2004. 23:723–725.
Article32. Rodríguez-Ares MT, Touriño R, López-Valladares MJ, Gude F. Multilayer amniotic membrane transplantation in the treatment of corneal perforations. Cornea. 2004. 23:577–583.
Article33. Chen KH, Hsu WM, Liang CK. Relapsing Mooren's ulcer after amniotic membrane transplantation combined with conjunctival autografting. Ophthalmology. 2004. 111:792–795.
Article34. Barros PS, Safatle AM, Godoy CA, Souza MS, Barros LF, Brooks DE. Amniotic membrane transplantation for the reconstruction of the ocular surface in three cases. Vet Ophthalmol. 2005. 8:189–192.
Article35. Arora R, Mehta D, Jain V. Amniotic membrane transplantation in acute chemical burns. Eye. 2005. 19:273–278.
Article36. Prabhasawat P, Tesavibul N. Preserved amniotic membrane transplantation for conjunctival surface reconstruction. Cell Tissue Bank. 2001. 2:31–39.37. Jain S, Rastogi A. Evaluation of the outcome of amniotic membrane transplantation for ocular surface reconstruction in symblepharon. Eye. 2004. 18:1251–1257.
Article38. Barabino S, Rolando M. Amniotic membrane transplantation in a case of ligneous conjunctivitis. Am J Ophthalmol. 2004. 137:752–753.
Article39. Dua HS, Gomes JA, King AJ, Maharajan VS. The amniotic membrane in ophthalmology. Surv Ophthalmol. 2004. 49:51–77.
Article40. Kim JC, Kim JH, Cheong TB. Amniotic membrane transplantation in perforation or impending perforation of cornea. J Korean Ophthalmol Soc. 1999. 40:1487–1495.41. Schechter BA, Rand WJ, Nagler RS, Estrin I, Arnold SS, Villate N, et al. Corneal melt after amniotic membrane transplant. Cornea. 2005. 24:106–107.
Article42. Jacob JT, Burgoyne CF, McKinnon SJ, Tanji TM, LaFleur PK, Duzman E. Biocompatibility response to modified Baerveldt glaucoma drains. J Biomed Mater Res. 1998. 43:99–107.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Filtering Operation Using Silicone Implant
- An Adhesion of Cartilage to Silicone Block using Histoacryl Glue
- Subconjunctival silicone oil drainage through the Molteno implant
- Conjunctival Necrosis following Ahmed Valve Implantation and Subtenon Triamcinolone Injection
- A Comparative study of the Implants used in the Management of Blowout Fracture