J Korean Med Sci.
2007 Sep;22(Suppl):S86-S90. 10.3346/jkms.2007.22.S.S86.
A Survey on the Impact of Operation Volume on Rectal Cancer Management
- Affiliations
-
- 1Department of Surgery, Korea University College of Medicine, Seoul, Korea.
- 2Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. sksohn@yumc.yonsei.ac.kr
- KMID: 1785794
- DOI: http://doi.org/10.3346/jkms.2007.22.S.S86
Abstract
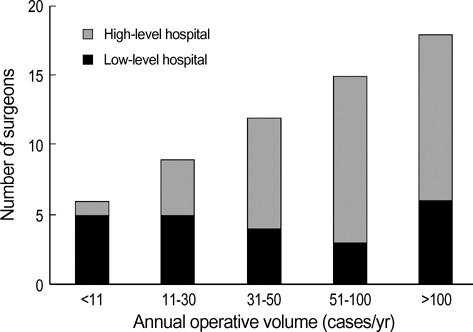
- The rectal cancer management can be influenced by the surgeon's practice and the hospital. This study was to evaluate the differences according to the surgeon's operative volume and the level of the hospital. Questionnaires were sent out to the members of the 'Korean Society of Coloproctology', and the responses were evaluated according to the surgeon's operation volume, the surgeon's age, and the level of the hospital. Sixty responses were received during the three months' period (from August to October 2004). Thirty three respondents (55%) operated more than 50 cases of rectal cancer per year (high-volume surgeons), and 37 respondents (61%) worked at university hospitals or tertiary care facilities (high-level hospitals). The preoperative evaluation with endorectal ultrasonography (ERUS) was significantly different according to the surgeon's operation volume and the level of the hospital, whereas magnetic resonance imaging and positron emission tomography (PET) was significantly different only for the surgeon's operation volume. The preoperative radiation therapy was significantly different according to the surgeon's operation volume, the surgeon's age, and the level of the hospital. However, there was no significant difference found on the operative procedures or postoperative surveillance. The preoperative loco-regional evaluation and the preoperative radiation therapy could be considered as the factors that influence the volume-outcome relationship in rectal cancer treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. MacFarlane JK, Ryall RD, Heald RJ. Mesorectal excision for rectal cancer. Lancet. 1993. 341:457–460.
Article2. Hool GR, Church JM, Fazio VW. Decision-making in rectal cancer surgery: survey of North American colorectal residency programs. Dis Colon Rectum. 1998. 41:147–152.3. Botterill ID, Blunt DM, Quirke P, Sebag-Montefiore D, Sagar PM, Finan PJ, Chalmers AG. Evaluation of the role of pre-operative magnetic resonance imaging in the management of rectal cancer. Colorectal Dis. 2001. 3:295–303.
Article4. Hermanek P, Hohenberger W. The importance of volume in colorectal cancer surgery. Eur J Surg Oncol. 1996. 22:213–215.
Article5. Harmon JW, Tang DG, Gordon TA, Bowman HM, Choti MA, Kaufman HS, Bender JS, Duncan MD, Magnuson TH, Lillemoe KD, Cameron JL. Hospital volume can serve as a surrogate for surgeon volume for achieving excellent outcomes in colorectal resection. Ann Surg. 1999. 230:404–411.
Article6. Schrag D, Panageas KS, Riedel E, Cramer LD, Guillem JG, Bach PB, Begg CB. Hospital and surgeon procedure volume as predictors of outcome following rectal cancer resection. Ann Surg. 2002. 236:583–592.
Article7. Meyerhardt JA, Tepper JE, Niedzwiecki D, Hollis DR, Schrag D, Ayanian JZ, O'Connell MJ, Weeks JC, Mayer RJ, Willett CG, Mac-Donald JS, Benson AB 3rd, Fuchs CS. Impact of hospital procedure volume on surgical operation and long-term outcomes in high-risk curatively resected rectal cancer: findings from the Intergroup 0114 Study. J Clin Oncol. 2004. 22:166–174.
Article8. McGrath DR, Leong DC, Gibberd R, Armstrong B, Spigelman AD. Surgeon and hospital volume and the management of colorectal cancer patients in Australia. ANZ J Surg. 2005. 75:901–910.
Article9. Glimelius B. Chemoradiotherapy for rectal cancer--is there an optimal combination? Ann Oncol. 2001. 12:1039–1045.10. Hannan EL, Wu C, Walford G, King SB 3rd, Holmes DR Jr, Ambrose JA, Sharma S, Katz S, Clark LT, Jones RH. Volume-outcome relationships for percutaneous coronary interventions in the stent era. Circulation. 2005. 112:1171–1179.
Article11. Kelly J, Tarnoff M, Shikora S, Thayer B, Jones DB, Forse RA, Hutter MM, Fanelli R, Lautz D, Buckley F, Munshi I, Coe N. Best practice recommendations for surgical care in weight loss surgery. Obes Res. 2005. 13:227–233.
Article12. Geubbels EL, Wille JC, Nagelkerke NJ, Vandenbroucke-Grauls CM, Grobbee DE, de Boer AS. Hospital-related determinants for surgical-site infection following hip arthroplasty. Infect Control Hosp Epidemiol. 2005. 26:435–441.
Article13. Ortholan C, Francois E, Thomas O, Benchimol D, Baulieux J, Bosset JF, Gerard JP. Role of radiotherapy with surgery for T3 and resectable T4 rectal cancer: evidence from randomized trials. Dis Colon Rectum. 2006. 49:302–310.
Article14. Kim NK, Kim MJ, Yun SH, Sohn SK, Min JS. Comparative study of transrectal ultrasonography, pelvic computerized tomography, and magnetic resonance imaging in preoperative staging of rectal cancer. Dis Colon Rectum. 1999. 42:770–775.
Article15. Garcia-Aguilar J, Pollack J, Lee SH, Hernandez de Anda E, Mellgren A, Wong WD, Finne CO, Rothenberger DA, Madoff RD. Accuracy of endorectal ultrasonography in preoperative staging of rectal tumors. Dis Colon Rectum. 2002. 45:10–15.
Article16. Mackay SG, Pager CK, Joseph D, Stewart PJ, Solomon MJ. Assessment of the accuracy of transrectal ultrasonography in anorectal neoplasia. Br J Surg. 2003. 90:346–350.
Article17. Bipat S, Glas AS, Slors FJ, Zwinderman AH, Bossuyt PM, Stoker J. Rectal cancer: local staging and assessment of lymph node involvement with endoluminal US, CT, and MR imaging--a meta-analysis. Radiology. 2004. 232:773–783.
Article18. Gearhart SL, Frassica D, Rosen R, Choti M, Schulick R, Wahl R. Improved staging with pretreatment positron emission tomography/ computed tomography in low rectal cancer. Ann Surg Oncol. 2006. 13:397–404.19. Lopez-Kostner F, Lavery IC, Hool GR, Rybicki LA, Fazio VW. Total mesorectal excision is not necessary for cancers of the upper rectum. Surgery. 1998. 124:612–617.
Article20. Law WL, Chu KW. Anterior resection for rectal cancer with mesorectal excision: a prospective evaluation of 622 patients. Ann Surg. 2004. 240:260–268.21. Phang PT. Total mesorectal excision: technical aspects. Can J Surg. 2004. 47:130–137.22. Gastinger I, Marusch F, Steinert R, Wolff S, Koeckerling F, Lippert H. Working Group 'Colon/Rectum Carcinoma'. Protective defunctioning stoma in low anterior resection for rectal carcinoma. Br J Surg. 2005. 92:1137–1142.
Article23. Wong NY, Eu KW. A defunctioning ileostomy does not prevent clinical anastomotic leak after a low anterior resection: a prospective, comparative study. Dis Colon Rectum. 2005. 48:2076–2079.
Article24. Park SM, Yun YH, Kwon S. Feasible economic strategies to improve screening compliance for colorectal cancer in Korea. World J Gastroenterol. 2005. 11:1587–1593.
Article25. Desch CE, Benson AB 3rd, Somerfield MR, Flynn PJ, Krause C, Loprinzi CL, Minsky BD, Pfister DG, Virgo KS, Petrelli NJ. American Society of Clinical Oncology. Colorectal cancer surveillance: 2005 update of an American Society of Clinical Oncology practice guideline. J Clin Oncol. 2005. 23:8512–8519.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correlation between tumor regression grade and rectal volume in neoadjuvant concurrent chemoradiotherapy for rectal cancer
- A Study of Anal Manometric Finding after Low Anterior Resection of Rectal Cancer
- Complete Rectal Prolapse Combined with Rectal Cancer: A Case Report
- Surgical issues in locally advanced rectal cancer treated by preoperative chemoradiotherapy
- Essential Items for Structured Reporting of Rectal Cancer MRI: 2016 Consensus Recommendation from the Korean Society of Abdominal Radiology