J Periodontal Implant Sci.
2010 Dec;40(6):271-275. 10.5051/jpis.2010.40.6.271.
Histologic evaluation of low-intensity pulsed ultrasound effects on bone regeneration in sinus lift
- Affiliations
-
- 1Department of Periodontology, Dankook University School of Dentistry, Cheonan, Korea. periohong@dankook.ac.kr
- KMID: 1783571
- DOI: http://doi.org/10.5051/jpis.2010.40.6.271
Abstract
- PURPOSE
Many techniques have been described for achieving vertical augmentation of the maxillary sinus. The aim of this study is to evaluate the effect of low-intensity pulsed ultrasound (LIPUS) to enhance bone regeneration after sinus floor elevation.
METHODS
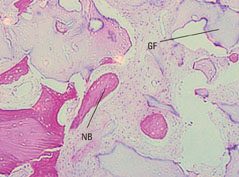
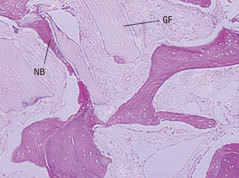
The sinus lifting technique was performed through a lateral approach on 8 different sites of 5 patients (3 males and 2 females) and their mean age was 45.7 years old. The sites were randomly assigned to the control or test groups. The control group had 4 sites that received lateral sinus lifting procedure only, while the test group had 4 sites that received LIPUS application after the lateral sinus lifting procedure. 24-32 weeks (an average of 29 weeks) postoperatively, new bone formation in the augmented sinus sites was evaluated through histologic and histomorphometric analyses of the biopsy specimens obtained during implant placement.
RESULTS
In the test group, the mean percentage of newly formed bone was 19.0+/-2.8%. In the control group, the mean percentage of newly formed bone was 15.2+/-3.1%. The percentage of newly formed bone was approximately 4% higher in those cases where the sinus was treated by LIPUS than the percentage in those cases where it was not used. The difference was statistically significant.
CONCLUSIONS
Within the scope of this study, low-intensity pulsed ultrasound application after sinus lifting appeared to have a significant effect on the development of new bone formation.
Keyword
MeSH Terms
Figure
Reference
-
1. Bays R. Pathophysiology and anatomy of edentulous bone loss. In : Fonseca RJ, Davis WH, editors. Reconstructive preprosthetic oral and maxillofacial surgery. Philadelphia: Saunders;1986. p. 1–17.2. Noack N, Willer J, Hoffmann J. Long-term results after placement of dental implants: longitudinal study of 1,964 implants over 16 years. Int J Oral Maxillofac Implants. 1999; 14:748–755.3. Smiler DG, Johnson PW, Lozada JL, Misch C, Rosenlicht JL, Tatum OH Jr, et al. Sinus lift grafts and endosseous implants: treatment of the atrophic posterior maxilla. Dent Clin North Am. 1992; 36:151–186.4. Khoury F. Augmentation of the sinus floor with mandibular bone block and simultaneous implantation: a 6-year clinical investigation. Int J Oral Maxillofac Implants. 1999; 14:557–564.5. Misch CE. Density of bone: effect on treatment plans, surgical approach, healing, and progressive boen loading. Int J Oral Implantol. 1990; 6:23–31.6. Sennerby L, Thomsen P, Ericson LE. A morphometric and biomechanic comparison of titanium implants inserted in rabbit cortical and cancellous bone. Int J Oral Maxillofac Implants. 1992; 7:62–71.7. Jemt T, Lekholm U. Oral implant treatment in posterior partially edentulous jaws: a 5-year follow-up report. Int J Oral Maxillofac Implants. 1993; 8:635–640.8. Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980; 38:613–616.9. Tatum H Jr. Maxillary and sinus implant reconstructions. Dent Clin North Am. 1986; 30:207–229.10. Wittbjer J, Palmer B, Rohlin M, Thorngren KG. Osteogenetic activity in composite grafts of demineralized compact bone and marrow. Clin Orthop Relat Res. 1983; (173):229–238.
Article11. Lindholm TS, Nilsson OS, Lindholm TC. Extraskeletal and intraskeletal new bone formation induced by demineralized bone matrix combined with bone marrow cells. Clin Orthop Relat Res. 1982; (171):251–255.
Article12. Sanders JJ, Sepe WW, Bowers GM, Koch RW, Williams JE, Lekas JS, et al. Clinical evaluation of freeze-dried bone allografts in periodontal osseous defects. Part III. Composite freeze-dried bone allografts with and without autogenous bone grafts. J Periodontol. 1983; 54:1–8.
Article13. Nasr HF, Aichelmann-Reidy ME, Yukna RA. Bone and bone substitutes. Periodontol 2000. 1999; 19:74–86.
Article14. Rosen PS, Reynolds MA, Bowers GM. The treatment of intrabony defects with bone grafts. Periodontol 2000. 2000; 22:88–103.
Article15. Hieu PD, Chung JH, Yim SB, Hong KS. A radiographical study on the changes in height of grafting materials after sinus lift: a comparison between two types of xenogenic materials. J Periodontal Implant Sci. 2010; 40:25–32.
Article16. Hatano N, Shimizu Y, Ooya K. A clinical long-term radiographic evaluation of graft height changes after maxillary sinus floor augmentation with a 2:1 autogenous bone/xenograft mixture and simultaneous placement of dental implants. Clin Oral Implants Res. 2004; 15:339–345.
Article17. Marx RE. Platelet-rich plasma (PRP): what is PRP and what is not PRP? Implant Dent. 2001; 10:225–228.
Article18. Gruber R, Varga F, Fischer MB, Watzek G. Platelets stimulate proliferation of bone cells: involvement of platelet-derived growth factor, microparticles and membranes. Clin Oral Implants Res. 2002; 13:529–535.
Article19. Lozada JL, Caplanis N, Proussaefs P, Willardsen J, Kammeyer G. Platelet-rich plasma application in sinus graft surgery: Part I--Background and processing techniques. J Oral Implantol. 2001; 27:38–42.
Article20. Boyapati L, Wang HL. The role of platelet-rich plasma in sinus augmentation: a critical review. Implant Dent. 2006; 15:160–170.
Article21. Takayama T, Suzuki N, Ikeda K, Shimada T, Suzuki A, Maeno M, et al. Low-intensity pulsed ultrasound stimulates osteogenic differentiation in ROS 17/2.8 cells. Life Sci. 2007; 80:965–971.
Article22. El-Bialy T, El-Shamy I, Graber TM. Repair of orthodontically induced root resorption by ultrasound in humans. Am J Orthod Dentofacial Orthop. 2004; 126:186–193.
Article23. Ding Y, Li G, Ao J, Zhou L, Ma Q, Liu Y. 99mTechnetium-methylene diphosphonate bone imaging using low-intensity pulsed ultrasound: promotion of bone formation during mandibular distraction osteogenesis in dogs. Br J Oral Maxillofac Surg. 2010; 48:94–99.
Article24. Smiler DG, Holmes RE. Sinus lift procedure using porous hydroxyapatite: a preliminary clinical report. J Oral Implantol. 1987; 13:239–253.25. Leung KS, Cheung WH, Zhang C, Lee KM, Lo HK. Low intensity pulsed ultrasound stimulates osteogenic activity of human periosteal cells. Clin Orthop Relat Res. 2004; (418):253–259.
Article26. Duarte LR. The stimulation of bone growth by ultrasound. Arch Orthop Trauma Surg. 1983; 101:153–159.
Article27. Dyson M, Brookes M. Stimulation of bone repair by ultrasound. Ultrasound Med Biol. 1983; Suppl 2. 61–66.28. Machen MS, Tis JE, Inoue N, Meffert RH, Chao EY, McHale KA. The effect of low intensity pulsed ultrasound on regenerate bone in a less-than-rigid biomechanical environment. Biomed Mater Eng. 2002; 12:239–247.29. Chapman IV, MacNally NA, Tucker S. Ultrasound-induced changes in rates of influx and efflux of potassium ions in rat thymocytes in vitro. Ultrasound Med Biol. 1980; 6:47–58.
Article30. Azuma Y, Ito M, Harada Y, Takagi H, Ohta T, Jingushi S. Low-intensity pulsed ultrasound accelerates rat femoral fracture healing by acting on the various cellular reactions in the fracture callus. J Bone Miner Res. 2001; 16:671–680.
Article31. Naruse K, Miyauchi A, Itoman M, Mikuni-Takagaki Y. Distinct anabolic response of osteoblast to low-intensity pulsed ultrasound. J Bone Miner Res. 2003; 18:360–369.
Article32. Wang SJ, Lewallen DG, Bolander ME, Chao EY, Ilstrup DM, Greenleaf JF. Low intensity ultrasound treatment increases strength in a rat femoral fracture model. J Orthop Res. 1994; 12:40–47.
Article33. Doan N, Reher P, Meghji S, Harris M. In vitro effects of therapeutic ultrasound on cell proliferation, protein synthesis, and cytokine production by human fibroblasts, osteoblasts, and monocytes. J Oral Maxillofac Surg. 1999; 57:409–419.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Brief Retrospect on the Use of Photobiomodulation (PBM) Therapy for Augmented Bone Regeneration (ABR)
- Enhanced Bone Regeneration by Bone Morphogenetic Protein-2 after Pretreatment with Low-Intensity Pulsed Ultrasound in Distraction Osteogenesis
- The Effect of Low-intensity Pulsed Ultrasound on Osteogenesis in Mini-pig Mandibles
- Stimulation of Fracture Healing in a Canine Ulna Full-defect Model by Low-intensity Pulsed Ultrasound
- Low-Intensity Pulsed Ultrasound Promotes BMP9 Induced Osteoblastic Differentiation in Rat Dedifferentiated Fat Cells