Korean J Radiol.
2005 Mar;6(1):31-36. 10.3348/kjr.2005.6.1.31.
Ductographic Findings of Breast Cancer
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine, Institute of Radiation Medicine, SNUMRC, and Clinical Research Institute, Seoul National University Hospital, Korea. nariya@radiol.snu.ac.kr
- 2Department of Radiology, Yonsei University College of Medicine, Korea.
- KMID: 1783170
- DOI: http://doi.org/10.3348/kjr.2005.6.1.31
Abstract
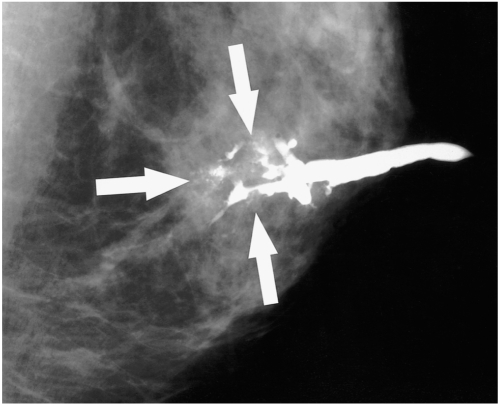
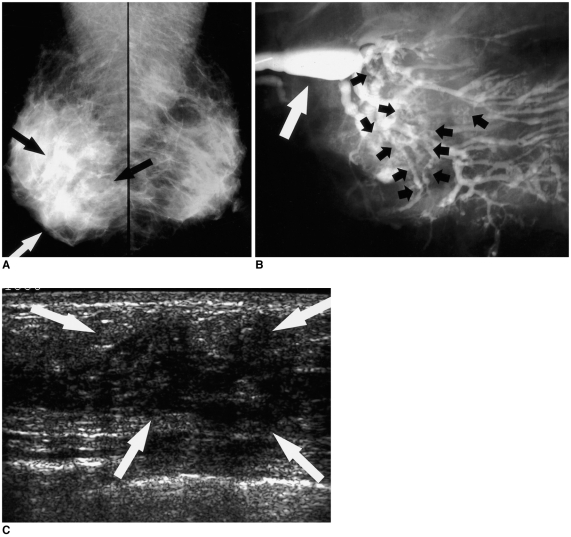
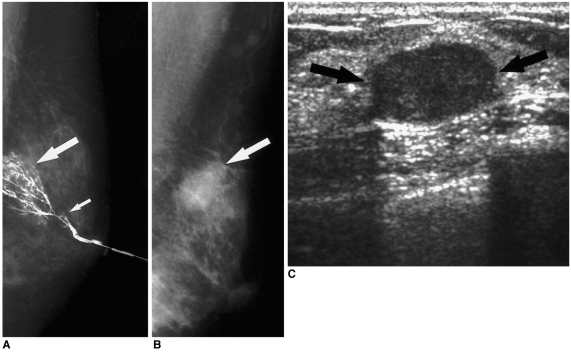
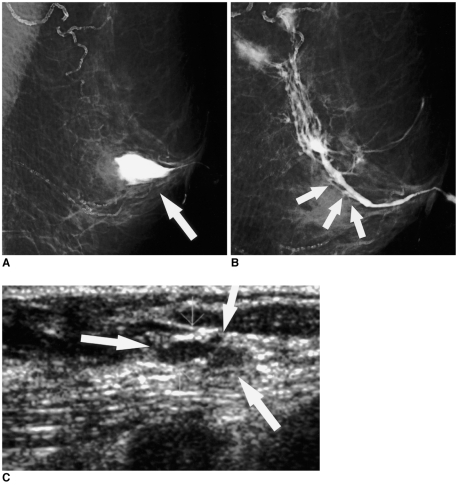
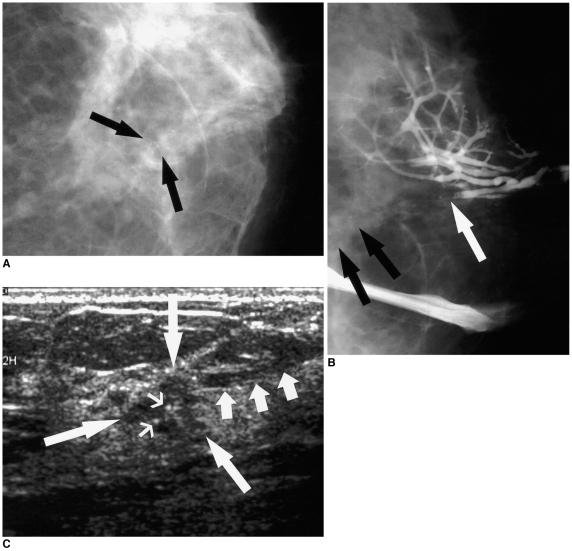
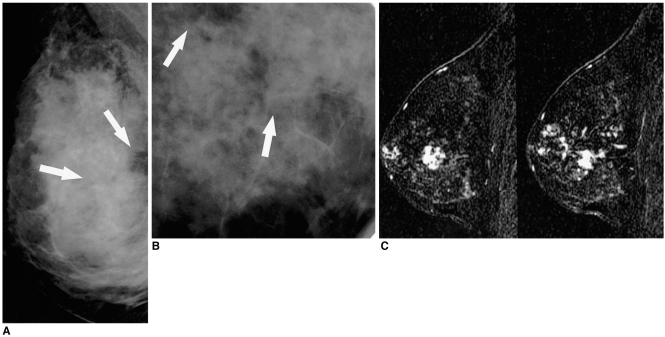
- Ductography has become the gold standard for the evaluation of patients exhibiting pathologic nipple discharges. In nine patients (age range, 29-67 years; median age, 51 years) with invasive (n=5) or intraductal (n=4) cancer, ductographic findings were recorded, then correlated with mammographic and sonographic findings. Common ductographic findings included complete ductal obstruction, multiple irregular filling defects in the nondilated peripheral ducts, ductal wall irregularities, periductal contrast extravasation, and ductal displacement. Faint microcalcifications or ill-defined masses, which were not opacified by contrast material, were often discovered adjacent to ductal abnormalities. Mammographically and sonographically occult diffusely spreading intraductal cancers often manifested as pathologic nipple discharge. In such cases, meticulous ductographic examinations and interpretations were crucial in order not to miss breast cancers.
MeSH Terms
Figure
Cited by 2 articles
-
Clinical Role of Breast Ultrasound
Nariya Cho, Woo Kyung Moon
J Korean Med Assoc. 2008;51(6):545-552. doi: 10.5124/jkma.2008.51.6.545.Conventional Galactography and MR Contrast Galactography for Diagnosing Nipple Discharge: Preliminary Results
Cüneyt Yücesoy, Emine Öztürk, Yusuf Özer, Tahsin Edgüer, Baki Hekimoglu
Korean J Radiol. 2008;9(5):426-431. doi: 10.3348/kjr.2008.9.5.426.
Reference
-
1. Tabar L, Dean PB, Pentek Z. Galactography: the diagnostic procedure of choice for nipple discharge. Radiology. 1983; 149:31–38. PMID: 6611939.
Article2. Sickles EA. Galactography and other imaging investigations of nipple discharge. Lancet. 2000; 356:1622–1623. PMID: 11089815.
Article3. Slawson SH, Johnson BA. Ductography: how to and what if? RadioGraphics. 2001; 21:133–150. PMID: 11158649.
Article4. Stavros AT. Stavros AT, editor. Nontargeted indications: breast secretions, nipple discharge, and intraductal papillary lesions of the breast. Breast ultrasound. 2004. 1st ed. Philadelphia, Pa: Lippincott Williams & Wilkins;p. 157–198.5. Moon WK, Myung JS, Lee YJ, Park IA, Noh DY, Im JG. US of ductal carcinoma in situ. RadioGraphics. 2002; 22:269–280. PMID: 11896217.
Article6. Chung SY, Lee KW, Park KS, Lee Y, Bae SH. Breast tumors associated with nipple discharge. Correlation of findings on galactography and sonography. Clin Imaging. 1995; 19:165–117. PMID: 7553430.
Article7. Cardenosa G, Doudna C, Eklund GW. Ductography of the breast: technique and findings. AJR Am J Roentgenol. 1994; 162:1081–1087. PMID: 8165986.
Article8. Hou MF, Huang TJ, Liu GC. The diagnostic value of galactography in patients with nipple discharge. Clin Imaging. 2001; 25:75–81. PMID: 11483413.
Article9. Cho N, Oh KK, Cho HY. Galactographic differentiation between malignant and benign disease in patients with pathologic nipple discharge. J Korean Radiol Soc. 2003; 48:511–516.
Article10. Chow JS, Smith DN, Kaelin CM, Meyer JE. Galactography-guided wire localization of an intraductal papilloma. Clin Radiol. 2001; 56:72–73. PMID: 11162702.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Highligts of 28th Annual Meeting of San Antonio Breast Cancer Symposium
- Surgery of Breast Cancer during the Last 5 Years: More Sophisticated and Specialized?
- Ultrasonographic Findings of Post-Operative Changes after Breast Cancer Surgery
- Ultrasonographic Findings of Postoperative Change after Breast Reconstruction
- Radiologic findings of male breast cancer: two cases report