J Korean Med Sci.
2006 Apr;21(2):290-294. 10.3346/jkms.2006.21.2.290.
Influence of Blood Lead Concentration on the Nerve Conduction Velocity in Patients with End-Stage Renal Disease
- Affiliations
-
- 1Department of Internal Medicine, Soonchunhyang University Cheonan Hospital, Cheonan, Korea. hwgil@schch.co.kr
- KMID: 1781837
- DOI: http://doi.org/10.3346/jkms.2006.21.2.290
Abstract
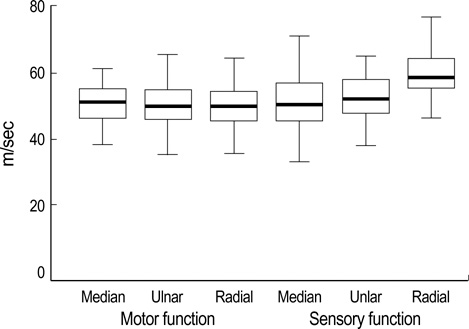
- Diseases of the peripheral nervous system are the most prevalent in patients with end-stage renal disease (ESRD). Although increased blood levels of lead in ESRD have been reported, the role of lead remains to be elucidated. The purpose of this study was to determine the connection of blood lead concentration with peripheral nerve conduction velocity. One hundred ninety-eight healthy subjects (control group) and 68 patients with ESRD undergoing hemodialysis (ESRD group) were enrolled. Nerve conduction was measured within two hours after hemodialysis. Orthodromic sensory nerve action potentials and compound muscle action potentials were recorded on the median, ulnar, and radial nerves. Hemoglobin-corrected blood lead was significantly higher in ESRD patients than in controls (9.1+/-2.8 microgram/dL vs. 5.9+/-2.3 microgram/dL, p<0.001). 32.4% of 68 ESRD patients with diabetes mellitus were significantly related to poorer motor and sensory nerve conduction velocity (p<0.001). However, blood lead was not a significant predictor of the nerve conduction velocity (p>0.05). Our result suggested that even though the blood lead levels were high in ESRD, they were not associated with the decline of peripheral nerve function. Diabetes mellitus is a primary independent risk of neuropathy in ESRD patients.
Keyword
MeSH Terms
-
Peripheral Nervous System Diseases/blood/etiology/physiopathology
Peripheral Nerves/physiopathology
Neural Conduction/*physiology
Middle Aged
Male
Lead/*blood/metabolism
Kidney Failure, Chronic/*blood/complications/*physiopathology
Humans
Female
Diabetic Neuropathies/blood/physiopathology
Case-Control Studies
Bone and Bones/metabolism
Body Burden
Adult
Figure
Reference
-
1. Nadig R. Goldfrank LR, editor. Lead. Toxicologic emergencies. 1994. Appleton and Lange;1029–1042.2. Robertson WO. Goldman L, Bennett JC, editors. Chronic poisoning: Trace metal and others. Cecil's Textbook of Medicine. 2000. W.B Saunders Co.;70–72.3. Batschelet E, Brand L, Steiner A. On the kinetics of lead in the human body. J Math Biol. 1979. 8:15–23.
Article4. Robinowitz M, Wetherill G, Kopple J. Lead metabolism in the normal human: stable isotope studies. Science. 1973. 182:725–727.
Article5. Silbergeld EK, Schwartz J, Mahaffey K. Lead and osteoporosis: mobilization of lead from bone in postmenopausal women. Environ Res. 1988. 47:79–94.
Article6. Keller CA, Doherty RA. Bone lead mobilization in lactating mice and lead transfer to suckling offspring. Toxicol Appl Pharmacol. 1980. 55:220–228.
Article7. Llach F, Bover J. Brenner BM, editor. Renal osteodystrophies. Brenner and Rector's The Kidney. 2000. W.B Saunders Co.;2103–2166.8. Hu H. Fauci AS, editor. Heavy metal poisoning. Harrison's Principles of Internal Medicine. 1998. McGraw-Hill Co.;2564–2566.9. Landrigan PJ. Strategies for epidemiologic studies of lead in bone in occupationally exposed populations. Environ Health Perspect. 1991. 91:81–86.
Article10. Denker BM, Chertow GM, Owen WF. Brenner BM, editor. Hemodialysis: neurologic abnormalities. Brenner and Rector's The Kidney. 2000. W.B Saunders Co.;2420–2421.11. Faster CL, Arieff AI. Schrier RW, Gottschalk CW, editors. Nervous system manifestations of renal failure. Diseases of the Kidney. 1993. Little Brown Co.;2789–2809.12. Nielsen VK. The peripheral nerve function in chronic renal failure. I. Clinical symptoms and signs. Acta Med Scand. 1971. 190:105–111.13. Kessler M, Durand PY, Hestin D, Cao Hun T, Renoult E, Prenat E, Chanliau J, Kaminski P, Duc M. Elevated body lead burden from drinking water in end-stage chronic lead failure. Nephrol Dial Transplant. 1995. 10:1648–1653.14. Van de Vyver FL, D'Haese PC, Visser WJ, Elseviers MM, Knippenberg LJ, Lamberts LV, Wedeen RP, De Broe ME. Bone lead in dialysis patients. Kidney Int. 1988. 33:601–607.
Article15. Kessler M, Durand PY, Hestin D, Gamberoni J, Chanliau J. Diagnosis and treatment of chronic lead poisoning in CAPD patients. Adv Perit Dial. 1993. 9:143–146.16. D'Haese PC, Couttenye MM, Lamberts LV, Elseviers MM, Goodman WG, Schrooten I, Cabrera WE, De Broe ME. Aluminum, iron, lead, cadmium, copper, zinc, chromium, magnesium, strontium, and calcium content in bone of end-stage renal failure patients. Clin Chem. 1999. 45:1548–1556.17. Kneip TJ, Crable JV. Methods for biological monitoring: a manual for assessing human exposure to hazardous substance. 1988. Washington DC: American Public Health Association;193–201.18. Thun M, Stayner L, Brown D, Waxweiler R. Mining and deaths from chronic renal failure. Lancet. 1982. 2:606.
Article19. Danilovic V. Chronic nephritis due to ingestion of lead contaminated flour. Br Med J. 1958. 29:27–28.20. Lilis R, Gavrilescu N, Nestorescu B, Dumitriu C, Roventa A. Nephropathy in chronic lead poisoning. Br J Ind Med. 1968. 25:196–202.
Article21. Jain VK, Cestero RV, Baum J. Carpal tunnel syndrome in patients undergoing maintenance hemodialysis. JAMA. 1979. 242:2868–2869.
Article22. Dumitru D. Dumitru D, editor. Generalized peripheral neuropathies. Electrodiagnostic Medicine. 1995. Hanley and Belfus Inc.;741–833.23. Bardin T, Zingraff J, Kuntz D, Drueke T. Dialysis related amyloidosis. Nephrol Dial Transplant. 1986. 1:151–154.24. van Ypersele de strihou C, Honhon B, Vandenbroucke JM, Huaux JP, Noel H, Maldague B. Dialysis amyloidosis. Adv Nephrol Necker Hosp. 1988. 17:401–421.25. Schwalbe S, Holzhauer M, Schaeffer J, Galanski M, Koch KM, Floege J. Beta(2)-microglobulin associated amyloidosis; a vanishing complication of long-term hemodialysis. Kidney Int. 1997. 52:1077–1083.26. Jadoul M, Garbar C, Vanholder R, Sennesael J, Michel C, Robert A, Noel H, van Ypersele de strihou C. Prevalence of histological beta-2-microglobulin amyloidosis in CAPD patients compared with hemodialysis patients. Kidney Int. 1998. 54:956–959.27. Zingraff J, Noel LH, Bardin T, Atienza C, Zins B, Drueke TB, Kuntz D. Beta-2-microglobulin amyloidosis in chronic renal failure [letter]. N Engl J Med. 1990. 323:1070–1071.28. Bolton CF, Driedger AA, Lindsay RM. Ischemic neuropathy in uremic patients caused by bovine arteriovenous shunt. J Neurol Neurosurg Psychiatry. 1979. 42:810–814.29. Fullerton PM. Chronic peripheral neuropathy produced by lead poisoning in guinea pigs. J Neuropathol Exp Neurol. 1966. 25:214–236.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Change of Autonomic and Peripheral Nerve Function after the First Twelve Months of Dialysis in End-stage Renal Disease
- Conduction Studies of the Saphenous Nerve in Normal Subjects and Patients with Femoral Neuropathy
- The Diagnostic Value of Segmental Nerve Conduction Study in Diabetics
- Motor Nerve Conduction Velocity in Newborn Infants and Children
- Nerve Conduction Study on Patients with Severe Liver Disease and Its Change after Transplantation