Ann Lab Med.
2013 Sep;33(5):331-342. 10.3343/alm.2013.33.5.331.
Variation in the Numbers of Red Blood Cell Units Transfused at Different Medical Institution Types from 2006 to 2010 in Korea
- Affiliations
-
- 1Department of Preventive Medicine, School of Medicine, Konkuk University, Seou, Korea. mubul@kku.ac.kr
- 2Department of Laboratory Medicine, School of Medicine, Konkuk University, Seoul, Korea.
- 3Department of Laboratory Medicine, School of Medicine, Yonsei University, Seoul, Korea.
- 4Division of Epidemic Intelligence Service, Korea Centers for Disease Control & Prevention, Osong, Korea.
- 5Division of Statistics, Graduate School of Public Health, Korea University, Seoul, Korea.
- KMID: 1781338
- DOI: http://doi.org/10.3343/alm.2013.33.5.331
Abstract
- BACKGROUND
This study aimed at assessing the number of red blood cell (RBC) units transfused at different types of medical institution and examining the characteristics of transfusion recipients.
METHODS
We calculated and compared the number of transfusion recipients, total RBC units transfused, and RBC units transfused per recipient. Study data were extracted from insurance benefits reimbursement claims for RBC units at the Health Insurance Review & Assessment Service from 2006 to 2010.
RESULTS
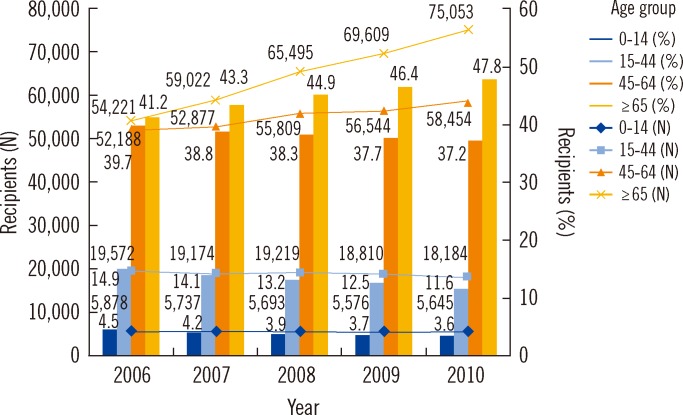
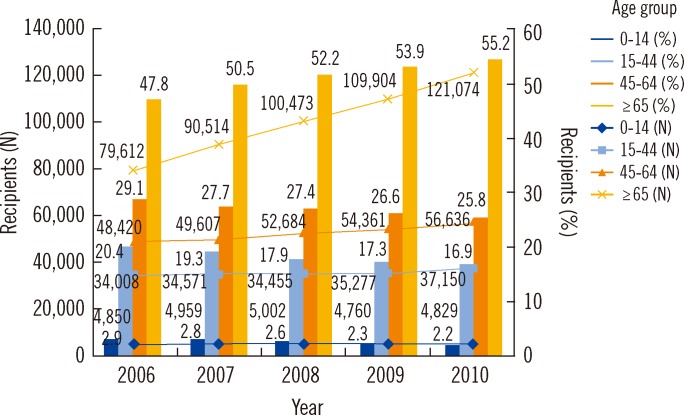
Between 2006 and 2010, the number of recipients of RBC units increased from 298,049 to 376,445, the number of RBC units transfused increased from 1,460,799 to 1,841,695, and the number of RBC units transfused per recipient changed from 4.90 to 4.89. The number of recipients aged > or =65 yr increased from 133,833 (44.9%) in 2006 to 196,127 (52.1%) in 2010. The highest number of RBC units was transfused to patients with neoplastic diseases (31.9%) and diseases of the musculoskeletal system and connective tissue (14.4%). More than 80% of the total number of RBC units were transfused at tertiary and general hospitals. However, this composition rate was slightly decreasing, with the composition rate for hospitals increasing from 12.6% to 16.3%.
CONCLUSIONS
This study revealed an increase in the number of RBC units transfused over a 5-yr period due to an increase in the number of transfused recipients, especially recipients aged > or =65 yr; moreover, the number of RBC units transfused differed based on medical institution type. These results provide fundamental data on RBC transfusions required for future research.
Keyword
MeSH Terms
-
Adolescent
Adult
Age Factors
Aged
Child
Child, Preschool
Connective Tissue Diseases/therapy
Databases, Factual
Erythrocyte Transfusion/*statistics & numerical data/*trends
Female
Hospitals, General/statistics & numerical data
Humans
Infant
Infant, Newborn
Insurance, Health, Reimbursement/*statistics & numerical data
Male
Middle Aged
Musculoskeletal Diseases/therapy
Neoplasms/therapy
Republic of Korea
Sex Factors
Tertiary Care Centers/statistics & numerical data
Young Adult
Figure
Cited by 1 articles
-
Patient Blood Management: An Internist's Perspective
Jieun Uhm
Hanyang Med Rev. 2018;38(1):38-48. doi: 10.7599/hmr.2018.38.1.38.
Reference
-
1. Korea Centers for Disease Control and Prevention. The monthly report for statics on blood supply (Dec. 2011). Cheongwon: KCDC;2012.2. United States Department of Health and Human Services. The 2007 national blood collection and utilization survey report. Washington, DC: DHHS;2009.3. United States Department of Health and Human Services. The 2009 national blood collection and utilization survey report. Washington, DC: DHHS;2011.4. Canadian Blood Services. A report to Canadian blood services 2008-2009: annual reports. Ottawa: CBS;2010. http://www.bloodservices.ca/CentreApps/Internet/UW_V502_MainEngine.nsf/resources/Annual+Reports/$file/CBS-Annual-Report-2008-2009-en.pdf.5. Australian Red Cross Blood Service. Annual reports 2009-2010. Melbourne: ARCBS;2011. Accessed 24 November 2012. Available from: http://www.donateblood.com.au/files/documents/ARCBS_AR_2010.pdf.6. Currie CJ, Patel TC, McEwan P, Dixon S. Evaluation of the future supply and demand for blood components in The United Kingdom National Health Service. Transfus Med. 2004; 14:19–24. PMID: 15043589.7. Regan F. New donors, new recipients-who gets what in 2003? Transfus Clin Biol. 2004; 11:53–56. PMID: 14980550.
Article8. Greinacher A, Fendrich K, Alpen U, Hoffmann W. Impact of demographic changes on the blood supply: Mecklenburg-West Pomerania as a model region for Europe. Transfusion. 2007; 47:395–401. PMID: 17319818.
Article9. Cobain TJ, Vamvakas EC, Wells A, Titlestad K. A survey of the demographics of blood use. Transfus Med. 2007; 17:1–15. PMID: 17266700.
Article10. Borkent-Raven BA, Janssen MP, van der Poel CL, Schaasberg WP, Bonsel GJ, van Hout BA. The PROTON study: profiles of blood product transfusion recipients in the Netherlands. Vox Sang. 2010; 99:54–64. PMID: 20202179.
Article11. Lim YA, Kwon SY, Park KU, Kwon SW. Survey of blood and blood components usages at ten university hospitals in Korea, 1995 to 2004. Korean J Blood Transfus. 2005; 16:197–208.12. Min HK, Kim HO. A survey of utilization of blood components for transfusion by training hospitals (2000). Korean J Blood Transfus. 2002; 13:135–141.13. Seo DH, Kwon SY, Kim DW, Jeon DS, Oh YC. Survey of blood and blood component utilization at eight university hospitals in Korea (1999). Korean J Blood Transfus. 2002; 13:143–148.14. Jeong EK. National blood policy for safe and adequate blood supply. J Korean Med Assoc. 2006; 49:416–422.
Article15. National Health Insurance Corporation & Health Insurance Review and Assessment Service. The 2006 National Health Insurance Statistical Yearbook. Seoul: Samwon Offset Printing;2007.16. National Health Insurance Corporation & Health Insurance Review and Assessment Service. The 2010 National Health Insurance Statistical Yearbook. Seoul: Sekwang Design Printing;2011.17. Korea National Statistical Office. Population Projections for Korea. Seoul: Korean National Statistical Office;2006. p. 1–56.18. Kim HS, Lee KS, Bae HJ, Koh IS, Chang SH, Im DH, et al. Changes in length of stay for neurological geriatric diseases in Korea between 2003 and 2007. J Clin Neurol. 2011; 7:148–155. PMID: 22087209.
Article19. Barr PJ, Donnelly M, Cardwell CR, Parker M, Morris K, Bailie KE. The appropriateness of red blood cell use and the extent of overtransfusion: right decision? right amount? Transfusion. 2011; 51:1684–1694. PMID: 21470238.
Article20. Hasley PB, Lave JR, Kapoor WN. The necessary and the unnecessary transfusion: a critical review of reported appropriateness rates and criteria for red cell transfusions. Transfusion. 1994; 34:110–115. PMID: 8310479.
Article21. Khanna MP, Hébert PC, Fergusson DA. Review of the clinical practice literature on patient characteristics associated with perioperative allogeneic red blood cell transfusion. Transfus Med Rev. 2003; 17:110–119. PMID: 12733104.
Article22. Joshi G, McCarroll M, O'Rourke P, Coffey F. Role of quality assessment in improving red blood cell transfusion practice. Ir J Med Sci. 1997; 166:16–19. PMID: 9057425.
Article23. Mold D, Allard S. P19 appropriateness of red cell transfusion in medical patients. Transfus Med. 2006; 16(S1):S32–S33.
Article24. Health Insurance Review Agency. HIRA quality assessment for institution based blood transfusion. J Korean Med Assoc. 2006; 49:402–409.25. Ministry of Health & Welfare. Korea Centers for Disease Control and Prevention. Korean Society of Blood Transfusion. 2011 Transfusion guideline. Cheongwon: KCDC;2011.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Guideline for the Order of Anticipated Red Cell Uses Incorporating Preoperative Patient's Variables for Elective Surgery
- Use of blood components, irradiated and filtered blood products in Chonnam University Hospital
- The Clinical Observation on the Volume of Blood Transfused during Anesthesia
- Incidence of Red Blood Cell Alloantibody Formation after Platelet Concentrate Transfusions
- Evaluation of Leukocyte Removal Efficiency of Prestorage Filter LeukoNet(TM)