Yonsei Med J.
2011 Mar;52(2):314-321. 10.3349/ymj.2011.52.2.314.
Cantilever Transforaminal Lumbar Interbody Fusion for Upper Lumbar Degenerative Diseases (Minimum 2 Years Follow Up)
- Affiliations
-
- 1Department of Orthopaedic Surgery, Bone, and Joint, Gifu University Graduate School of Medicine, Gifu, Japan.
- 2Department of Reconstructive Surgery for Spine, Bone, and Joint, Gifu University Graduate School of Medicine, Gifu, Japan. kei@bg8.so-net.ne.jp
- KMID: 1779669
- DOI: http://doi.org/10.3349/ymj.2011.52.2.314
Abstract
- PURPOSE
To evaluate the clinical outcomes of cantilever transforaminal lumbar interbody fusion (c-TLIF) for upper lumbar diseases.
MATERIALS AND METHODS
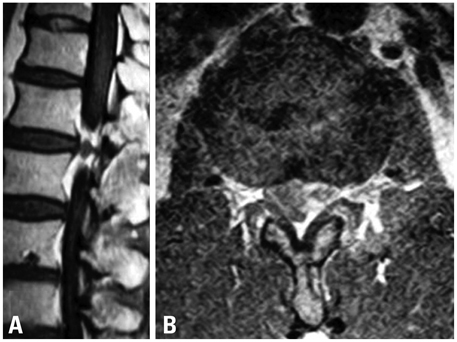
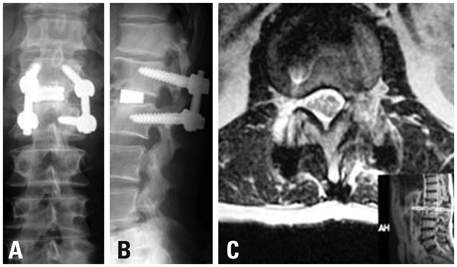
Seventeen patients (11 males, 6 females; mean +/- SD age: 62 +/- 14 years) who underwent c-TLIF using kidney type spacers between 2002 and 2008 were retrospectively evaluated, at a mean follow-up of 44.1 +/- 12.3 months (2 year minimum). The primary diseases studied were disc herniation, ossification of posterior longitudinal ligament (OPLL), degenerative scoliosis, lumbar spinal canal stenosis, spondylolisthesis, and degeneration of adjacent disc after operation. Fusion areas were L1-L2 (5 patients), L2-L3 (9 patients), L1-L3 (1 patient), and L2-L4 (2 patients). Operation time, blood loss, complications, Japanese Orthopaedic Association (JOA) score for back pain, bone union, sagittal alignment change of fusion level, and degeneration of adjacent disc were evaluated.
RESULTS
JOA score improved significantly after surgery, from 12 +/- 2 to 23 +/- 3 points (p < 0.01). We also observed significant improvement in sagittal alignment of the fusion levels, from - 1.0 +/- 7.4 to 5.2 +/- 6.1 degrees (p < 0.01). Bony fusion was obtained in all cases. One patient experienced a subcutaneous infection, which was cured by irrigation. At the final follow-up, three patients showed degenerative changes in adjacent discs, and one showed corrective loss of fusion level.
CONCLUSION
c-TLIF is a safe procedure, providing satisfactory results for patients with upper lumbar degenerative diseases.
Keyword
MeSH Terms
-
Adult
Aged
Back Pain/surgery
Blood Loss, Surgical
Female
Follow-Up Studies
Humans
Intervertebral Disk Displacement/surgery
Lumbar Vertebrae/*surgery
Male
Middle Aged
Scoliosis/surgery
Spinal Diseases/*surgery
Spinal Fusion/adverse effects/*methods
Spinal Stenosis/surgery
Spondylolisthesis/surgery
Time Factors
Treatment Outcome
Figure
Reference
-
1. Albert TJ, Balderston RA, Heller JG, Herkowitz HN, Garfin SR, Tomany K, et al. Upper lumbar disc herniations. J Spinal Disord. 1993. 6:351–359.
Article2. Aronson HA, Dunsmore RH. Herniated upper lumbar discs. J Bone Joint Surg Am. 1963. 45:311–317.
Article3. Bosacco SJ, Berman AT, Raisis LW, Zamarin RI. High lumbar disc herniations. Case reports. Orthopedics. 1989. 12:275–278.4. Cloward RB. The treatment of ruptured lumber intervertebral discs by vertebral body fusion. I. Indications, operative technique, after care. J Neurosurg. 1953. 10:154–168.
Article5. Brantigan JW, Steffee AD, Lewis ML, Quinn LM, Persenaire JM. Lumbar interbody fusion using the Brantigan I/F cage for posterior lumbar interbody fusion and the variable pedicle screw placement system: two-year results from a Food and Drug Administration investigational device exemption clinical trial. Spine (Phila Pa 1976). 2000. 25:1437–1446.
Article6. Shin HC, Yi S, Kim KN, Kim SH, Yoon do H. Posterior lumbar interbody fusion via a unilateral approach. Yonsei Med J. 2006. 47:319–325.
Article7. Elias WJ, Simmons NE, Kaptain GJ, Chadduck JB, Whitehill R. Complications of posterior lumbar interbody fusion when using a titanium threaded cage device. J Neurosurg. 2000. 93:45–52.
Article8. Ido K, Shimizu K, Tada H, Matsuda Y, Shikata J, Nakamura T. Considerations for surgical treatment of patients with upper lumbar disc herniations. J Spinal Disord. 1998. 11:75–79.
Article9. Harms J, Rolinger H. [A one-stage procedure in operative treatment of spondylolistheses: dorsal traction-reposition and anterior fusion (author's transl)]. Z Orthop Ihre Grenzgeb. 1982. 120:343–347.10. Humphreys SC, Hodges SD, Patwardhan AG, Eck JC, Murphy RB, Covington LA. Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine (Phila Pa 1976). 2001. 26:567–571.
Article11. Lowe TG, Tahernia AD. Unilateral transforaminal posterior lumbar interbody fusion. Clin Orthop Relat Res. 2002. 394:64–72.
Article12. Anand N, Hamilton JF, Perri B, Miraliakbar H, Goldstein T. Cantilever TLIF with structural allograft and RhBMP2 for correction and maintenance of segmental sagittal lordosis: long-term clinical, radiographic, and functional outcome. Spine (Phila Pa 1976). 2006. 31:E748–E753.13. Moskowitz A. Transforaminal lumbar interbody fusion. Orthop Clin North Am. 2002. 33:359–366.
Article14. Lowe TG, Tahernia AD, O'Brien MF, Smith DA. Unilateral transforaminal posterior lumbar interbody fusion (TLIF): indications, technique, and 2-year results. J Spinal Disord Tech. 2002. 15:31–38.
Article15. Hioki A, Miyamoto K, Kodama H, Hosoe H, Nishimoto H, Sakaeda H, et al. Two-level posterior lumbar interbody fusion for degenerative disc disease: improved clinical outcome with restoration of lumbar lordosis. Spine J. 2005. 5:600–607.
Article16. Hee HT, Castro FP Jr, Majd ME, Holt RT, Myers L. Anterior/posterior lumbar fusion versus transforaminal lumbar interbody fusion: analysis of complications and predictive factors. J Spinal Disord. 2001. 14:533–540.
Article17. Cutler AR, Siddiqui S, Mohan AL, Hillard VH, Cerabona F, Das K. Comparison of polyetheretherketone cages with femoral cortical bone allograft as a single-piece interbody spacer in transforaminal lumbar interbody fusion. J Neurosurg Spine. 2006. 5:534–539.
Article18. Whitecloud TS 3rd, Roesch WW, Ricciardi JE. Transforaminal interbody fusion versus anterior-posterior interbody fusion of lumbar spine: a financial analysis. J Spinal Disord. 2001. 14:100–103.
Article19. Hackenberg L, Halm H, Bullmann V, Vieth V, Schneider M, Liljenqvist U. Transforaminal lumbar interbody fusion: a safe technique with satisfactory three to five year results. Eur Spine J. 2005. 14:551–558.
Article20. Rosenberg WS, Mummaneni PV. Transforaminal lumbar interbody fusion: technique, complications, and early results. Neurosurgery. 2001. 48:569–574.
Article21. Etebar S, Cahill DW. Risk factors for adjacent-segment failure following lumbar fixation with rigid instrumentation for degenerative instability. J Neurosurg. 1999. 90:163–169.
Article22. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976). 2004. 29:1938–1944.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Uniportal Endoscopic Lumbar Interbody Fusion
- Biportal Endoscopic Transforaminal Lumbar Interbody Fusion with Percutaneous Instrumentation: A Technical Note
- Minimally Invasive Lateral Lumbar Interbody Fusion: Indications, Outcomes and Complications
- Radiographic Results of Single Level Transforaminal Lumbar Interbody Fusion in Degenerative Lumbar Spine Disease: Focusing on Changes of Segmental Lordosis in Fusion Segment
- Biportal Endoscopic Transforaminal Lumbar Interbody Fusion with Arthroscopy